Recommended

CGD NOTES
We would like to acknowledge Oliver Johnson for valuable advice and feedback on this work.
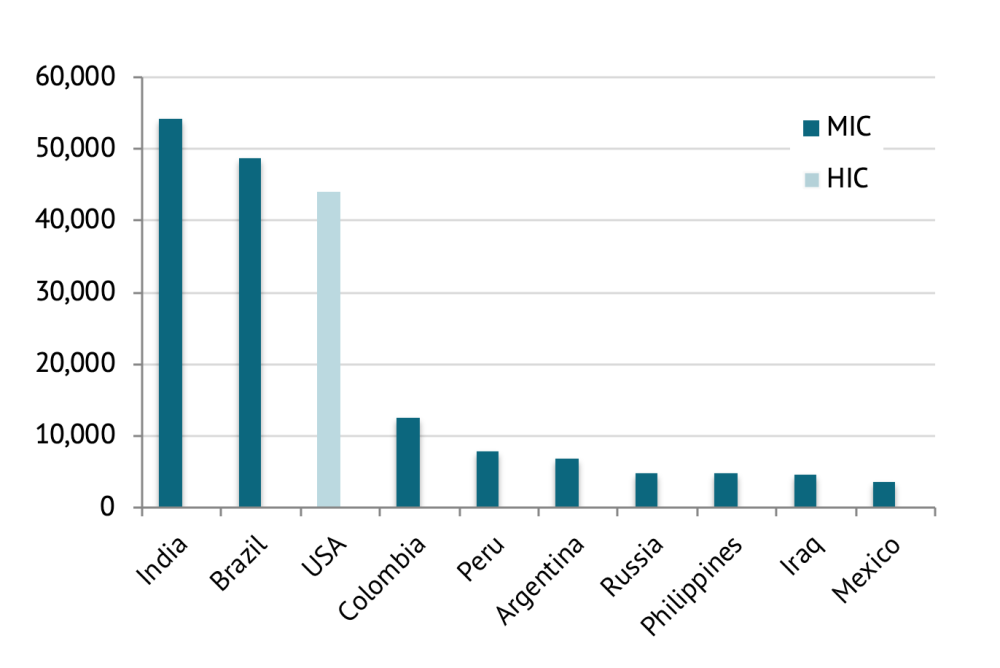
As high-income countries in Europe continue to see improvements in the number of new cases, hospitalizations and deaths from COVID-19 outbreaks in middle-income countries (MICs) have started to surge. After the United States, large MICs such as India, Brazil, Russia, and South Africa lead the world in the total number of COVID-19 cases. Nine of the top 10 countries for new daily cases are MICs (figure 1). The global public health response to COVID-19 is pivoting from high-income European countries to MICs predominantly in Asia and South America.
Figure 1. New COVID-19 cases reported (18 August 2020), by country
Effective test, trace, and isolate (TTI) systems have featured alongside other measures in a number of high-income countries, such as South Korea and Taiwan. Such strategies can be more efficient than mass testing or screening approaches under certain circumstances. Modellers have found that targeted contact tracing would mitigate the risk of a second wave at just a fraction of the cost of large lockdowns. TTI systems may therefore be particularly valuable in MICs, where social and economic circumstances do not support large and long-term lockdowns. But investing in such systems in MICs comes with a number of limitations and opportunity costs. To make the most of a national TTI system, decision-makers will need to understand its role in different phases of an epidemic, and, alongside wider health objectives, consider local and regional inequity in the availability of resources, and optimise its constituent parts (i.e., testing, contact tracing, and isolation).
Here, we present seven key recommendations for COVID-19 test, trace and isolate systems, accounting for the specific context of MICs:
Use TTI alongside other public health interventions as part of a layered approach to disease control, focussing limited resources on new clusters and high-risk settings during the peak of an epidemic.
Build TTI systems around unified public health objectives that go beyond COVID-19 alone, recognising pre-existing health needs as well as those exacerbated by the crisis.
Standardise the impact of TTI systems at a subnational level through targeted investment in health system strengthening, emergency preparedness, disease surveillance, and public health education.
Ration tests through the use of pooled testing where the pre-test odds of COVID-19 are low, and syndromic surveillance systems where the pre-test odds of COVID-19 are high.
Minimise financial and social barriers to testing, with tests paid for by governments in populations that are vulnerable to catastrophic health expenditures.
Invest in the recruitment and retention of community health workers for manual contact tracing, ensuring sufficient public engagement to encourage participation and to build trust in public health institutions.
Provide voluntary financial, humanitarian, and accommodation support to enable vulnerable cases (and contacts) to isolate effectively where otherwise not possible.
The middle-income context
MICs make up a large and heterogeneous group of countries with varying population demographics, economies, systems of governance, social norms, cultures, and health systems. Nonetheless, they share many common characteristics that make them different from both high- and low-income countries, and especially vulnerable to COVID-19. MICs as a group are home to three-quarters of the world’s population and 62 percent of the world’s poor, with many living in slums and informal settlements. Cities are typically densely populated, with growing, young, urban, mobile, and unequal populations. MICs account for about one-third of global GDP, with large informal sectors that drive global economic growth. Globally, obesity was responsible for approximately 8 percent of deaths in 2017, but in MICs this figure was almost double at 15 percent. Cardiovascular disease, hypertension, and diabetes, associated with COVID-19 disease severity, are also concentrated in MICs. This presents a challenge for COVID-19 control in otherwise young and relatively low-risk populations.
Most MICs are accustomed to infectious diseases. With unequal development, many populations within MICs remain in the early stages of the epidemiological transition, where infectious diseases are still the major cause of death. Outbreak response and disease surveillance systems are therefore well established in many MICs. In China for instance, technology was already firmly embedded into the health protection system, meaning when COVID-19 arrived, authorities were quickly able to track people’s movements over time. Using personal data, WeChat and Alipay released colour-based QR codes to aid outbreak response: green for “safe,” yellow requiring a seven-day quarantine, and red for a 14-day quarantine. Not all MICs have had a similar experience with technology, but some MIC TTI systems may be supported by favourable social attitudes to infectious disease. A YouGov public opinion survey across 25 countries found that those living in Asia were more fearful of catching COVID-19, and the pandemic had a greater impact on behaviour (including hygiene, wearing facemasks, and avoiding crowded areas), compared to populations in Europe and North America. Although not all MICs will be in the same position, those in Asia may find that these sociocultural factors can be mobilized to enhance the successful implementation of their TTI systems through public participation, extensive data sharing, and compliance with guidance.
When to test, trace, and isolate?
TTI on its own cannot be relied upon to keep the virus’s reproduction number (or R value) below 1, as it will struggle to keep up when cases are growing exponentially. The Africa CDC support the use of contact tracing in the initial phases of an epidemic, but not in the later phases where there is widespread nationwide transmission. The World Health Organization (WHO) reiterates this message, suggesting that contact tracing is of limited use when disease transmission is intense. They do not recommend halting TTI altogether, but rather focussing on low-prevalence areas and high-risk settings. In the UK, contact tracing was abandoned after community transmission outstripped existing resources but reinstituted after case numbers became more manageable. Many MICs will face a similar scenario where resources are eventually stretched. Research suggests that the transmissibility of SARS-COV-2 is highly variable, with as much as 80 percent of spread driven by as few as 10 percent of cases. Dynamic TTI systems informed by real-time data can therefore be effective by directing resources to areas with new outbreaks and clusters where containment may still be possible, as well as those in high-risk indoor settings.
Many high-income countries once past the peak transitioned away from nationwide lockdowns, becoming more reliant on dynamic local systems, including TTI. Finding the equilibrium between large-scale restrictive public health interventions and more targeted measures like TTI, once past the peak, will be particularly challenging for MICs. Even in the absence of lockdowns, the burden on TTI systems in high-income countries has been greatly lessened through social distancing. Where social distancing is well practiced, those who are positive for COVID-19 will have few close contacts that require identification and isolation. In the favelas, home to around 13 million Brazilians, social distancing and hand washing are virtually impossible. TTI systems therefore, whilst advisable in all countries, may prove less sustainable in MICs, in the absence of other public health interventions to help restrict close contact. A layered approach to COVID-19 control will be especially important whilst emerging from the peak of an epidemic, where MICs must be wary of complacency and over-reliance on local TTI systems.
Developing unified public health objectives
The major problem with scaling up TTI systems is the opportunity cost of diverting resources away from other essential public health programmes and healthcare services. The budget of the UK test and trace programme is £10 billion. In MICs, this scale of investment may be unpalatable. Kenya has already moved away from TTI, with limited testing due to the costs associated with scaling up capacity. Any investment in a new disease-specific public health programme could take resources away from others, like health education, screening, WASH, and vaccination. According to a UNICEF, WHO, and GAVI pulse survey, three-quarters of the 82 countries that responded reported COVID-19-related disruptions in their immunization programmes as of May 2020. Even other outbreak response activities are at risk if TTI systems are too narrow in their remit. In April, the Ghana Health Service reported at least 409 cases of meningitis in five regions, with 40 deaths. Investigation showed that the high fatality was due to late reporting of cases, since the government was so focussed on COVID-19 alone.
The demand for essential public health services in MICs is greater than ever. Siphoning resources into a narrow and vertically organized COVID-19 response could further endanger these escalating public health needs. Given what we know about the risk of severe illness in COVID-19, public health programmes focussing on obesity, smoking, non-communicable diseases, malnutrition, and infectious diseases other than COVID-19 will be fundamentally critical in mitigating the impact of COVID-19. Developing unified objectives that consider COVID-19 against the backdrop of routine public health and healthcare services, as well as pandemic-related changes in health needs, is both possible and required. For many, a new and improved TTI system could be directly used in the health protection response for other common infectious diseases. Plans in the UK for new swab tests, deployed through TTI, can detect influenza as well as COVID-19: undoubtedly helpful in limiting the transmission of both diseases simultaneously. To address the rising burden of non-communicable diseases in MICs, suspected COVID-19 patients identified through TTI could also be risk-stratified, and then educated, screened, or tested for conditions like cardiovascular disease and cancer. Broadening the remit of TTI systems to go beyond COVID-19 alone offers an opportunity to positively engage with the young individuals in MICs with poor health-seeking behaviour, who might otherwise be unknown to public health or healthcare services.
Standardising subnational implementation of TTI
TTI is a community-centred system that relies on accessible and high-quality public health systems, as well as wider health, education and communications infrastructure. Data from the UN Development Programme (UNDP) shows that when measuring the ratio of the average income of the richest 20 percent to the poorest 20 percent, the top five countries globally are middle-income. The same can be said when using the GINI index to measure income inequality. With wealth inequality and variable investment in healthcare, education, and infrastructure a longstanding issue for many MICs, TTI systems are unlikely to be uniformly effective across nations. Some argue that the wealthier provinces in South Africa, like Western Cape, are at an advantage over others in having the infrastructure required to an enable TTI to be effective.
In India, Kerala has been better placed compared to other states in managing the COVID-19 pandemic. It has historically been considered a wealthy state with one of the highest literacy rates and best health systems in India. In the last few years Kerala had a major flood and the Nipah virus outbreak. The state learned from these experiences and accordingly invested in emergency preparedness and disease surveillance mechanisms. The state registered India’s first COVID-19 case on 30 January 2020 and was the first to declare a health emergency and start TTI. Strong existing health systems (both primary and secondary care) as well as widespread community participation have been vital in facilitating the success of TTI in Kerala. The state of Bihar on the other hand is historically one of the poorest in India, with a relatively weak health system. Since 1995, Bihar state has encountered disease outbreaks like acute encephalitis syndrome in Muzaffarpur and annual floods. Despite this, there has been relatively limited application of this learning to strengthen disease surveillance, emergency preparedness, and health system infrastructure and governance. Bihar has therefore struggled to put in place an effective TTI system and is now at risk of encountering a tsunami of COVID infections.
The long-term sustainability of TTI will depend upon successful implementation in all regions, not just the most affluent. This will require national coordination and targeted investment in health system strengthening, emergency preparedness, disease surveillance, and public health education. Without this broad and concerted effort, TTI systems are likely to fail in some regions and succeed in others: magnifying large existing health inequalities in MICs that have already been deeply exploited by COVID-19.
Optimising the TTI system
Table 1 displays the various factors involved in optimising each component of a TTI system, with discussion below.
Table 1. Optimising the components of test and trace systems in MICs
| Test | Trace | Isolate |
|---|---|---|
| Eligibility: standardized criteria for testing and prioritisation based on strategic goals (e.g. vulnerable populations, healthcare workers) | Public health workforce: recruit contact tracers or community health workers, train to identify cases and contacts as well as provide public health guidance and decision-making, with adequate access to PPE and professional incentives | Environment: increase financial protection and ensure targeted housing/humanitarian support for effective isolation and quarantine in high-risk populations |
| Acceptability: minimise social stigma associated with a positive test and improve engagement with communities sceptical of modern medical practice | Technology: invest in scaling up mobile technology to help identify unknown contacts in densely populated areas and integrate with manual tracing systems | Monitoring: encourage and monitor compliance to isolation measures e.g. through employers, community engagement, and feedback mechanisms |
| Turnaround time: invest in rapid diagnostic tests where available, consider pooled testing, and invest in infrastructure to support the transport of specimens across large areas/remote terrain, the laboratory processing of specimens, and rapid reporting of results | Communications: clear, standardized advice on actions after identified as contact and regularly updated guidance for all affected sectors/employers | Legislation: use of legislation where required to enforce disease control measures, but with unambiguous triggers and systems of accountability to prevent abuse and promote public trust in institutions |
| Affordability: minimise out-of-pocket payments for tests, with government to cover costs for those at risk of catastrophic expenditure, and ensure quality of test offered is not based on price | Public trust and participation: encourage data sharing and strengthen confidence in local public health institutions through community engagement, clear public health messaging, protecting privacy, accountability, and transparency |
Test
Two key tests have emerged in the pandemic: the PCR assay, which identifies current infection through detecting viral RNA, and the antibody test, which detects antibodies that are created from an immune response to previous infection. For the purposes of TTI and with limited knowledge on the role of antibodies in long-term immunity, expanding PCR capacity has been the cornerstone of pandemic response in high-income countries. Shortages in PCR testing have been observed in most MICs. At the end of May, South Africa faced a backlog of more than 96,000 unprocessed cases awaiting coronavirus tests, according to the health ministry.
One possible solution to limited PCR testing capacity is pooled sampling such as that seen in Ghana. Instead of testing one person at a time, samples from multiple individuals are put together and tested as one pool. Each pool has 10 samples and 100 pools are tested at a time. If the pooled test comes back negative, everyone in the pool is declared negative. But if it is positive, each member of the pool is then retested individually. This approach enabled test turnaround times to come down from around six days to just two. For MICs, pooled testing could therefore increase the impact of TTI when the prevalence of COVID-19 is low. In India, a PCR test positivity rate of over 5 percent is the threshold at which guidance from the Indian Council for Medical Research (ICMR) considers the prevalence of COVID-19 to be too high for this strategy to be useful.
Another method to reduce lengthy turnaround times and increase the availability of testing in MICs is through rapid diagnostic tests (RDTs). RDTs can be deployed at a local level, with rapid results at a low cost. Although emerging RDTs have mostly failed to meet quality standards, there are some that have shown promising results. For instance, the SD BioSensor Rapid Antigen Test displays reasonably high sensitivity across different studies, and is one of the two rapid antigen tests currently approved by the Indian ICMR.
In recognition of testing shortages and the subsequent impact on the rest of the TTI system, there have been calls for suspected COVID-19 cases, diagnosed clinically in the community or in hospital, to form part of TTI systems. Tracing the contacts of suspected cases (rather than confirmed) can be much quicker and therefore more effective for disease control, since individuals are thought to be most infectious around the time of symptom onset. The major risk of such systems built around syndromic surveillance is that they can lead to unnecessary isolation, anxiety, and testing, since many will be incorrectly identified as close contacts. This strategy would be particularly inefficient as the background incidence of similar acute respiratory infections (such as influenza) increases, and the prevalence of COVID-19 falls. It could, however, be a valuable tool for MICs attempting to operate a TTI system in the peak of an epidemic.
Unlike in most high-income countries, the majority of tests have been completed in the private sector in South Africa. With the global economic downturn arising from COVID-19, cost remains an important barrier to testing where public sector capacity and insurance schemes are limited. Out-of-pocket expenditure as a percentage of all health expenditure in Nigeria was 77.2 percent in 2017, one of the highest levels in the world. High pre-existing out-of-pocket health expenditures in MICs combined with the catastrophic economic fallout of the pandemic in vulnerable low-income populations puts COVID-19 testing at risk. Many may prioritise saving for expensive treatment over testing in an early stage of illness. Out-of-pocket expenditure can be minimised through state regulation of the private sector, as in India, where private diagnostic providers were capped at Rs 4500 per test. Chile similarly established a maximum cost of USD 30 for the COVID-19 test in private healthcare facilities. Whether through engaging the private sector or expanding public sector services, financial barriers to testing must be minimised for TTI systems to function across MIC populations.
In addition to financial barriers, governments must reduce the social barriers associated with COVID-19 that can act as a barrier to testing. Social stigma, discrimination, and exclusion have been described in detail in other infectious diseases (e.g., tuberculosis, HIV/AIDS) and COVID-19 has been no different. In March, WHO stated, “some healthcare workers may unfortunately experience avoidance by their family or community owing to stigma or fear.” A COVID-19 survivor in Harare, Zimbabwe was surprised when the road in front of his house was named “corona road” and some avoided it fearing the possibility of infection.
The concern of being discriminated against, and resulting delays in testing, can lead to two hazardous clinical and public health consequences: delayed presentation of symptomatic patients to healthcare services and under-detection of infectious individuals (resulting in increased viral transmission to susceptible contacts). People with greater personal resources (income, education, social support) and good mental health have been shown to be less likely to stigmatise. Education, clear and honest communication, and the use of non-discriminatory language have the potential to significantly reduce the social stigma related to COVID-19, minimise barriers to testing, and thereby improve the utility of TTI systems.
Trace
Countries have taken different approaches in where the responsibility for contact tracing lies. In Norway, GPs rather than local public health teams are responsible for tracing contacts of confirmed COVID-19 cases. For MICs, community health workers (CHWs) are often the first point of contact for vulnerable and underserved populations. CHWs often conduct contract tracing and support isolation: robust networks of CHWs may be one of the many reasons why some countries were initially successful in mitigating the spread of COVID-19. In many high-income countries contact tracing is largely done remotely via telephone and email. Large cities in MICs are rife with informal settlements and sparsely populated rural areas that lack an adequate communications infrastructure. Local teams with “feet on the ground” are essential.
Because of this reliance on community presence, personal protective equipment (PPE) is critical for the effective expansion of TTI systems in MICs. PPE deficits have affected all health workers, but recent evidence suggests CHWs have been disproportionately affected due, in large part, to their incomplete integration within national health systems. Beyond PPE, providing allowances for housing and transport, equal training opportunities, adequate salaries (paid on time and for a broad range of services) and awards in high-profile public events have been shown to contribute to better recruitment and retention of CHWs.
Automated digital tools can help to identify the unknown contacts of those with COVID-19, thereby bolstering manual contact tracing efforts. Digital proximity-tracking tools, although useful, will be insufficient as a lone tool in MICs, with large numbers of people who lack access to mobiles and Internet. Aaroyga Setu in India has had approximately 130 million downloads to date, representing only around 10 percent of the Indian population. Mobile phone coverage aside, manual contact tracing that involves members of the public speaking to local public health teams can be more effective than other methods. Researchers from the University of Oxford found that app-based tracing achieved a 44 percent reduction in transmission, whereas manual tracing reduced transmission by 61 percent, on the assumption that 53 percent of the population would use the contact tracing app.
Community buy-in is a prerequisite for effective contact tracing, which relies on individuals voluntarily providing detailed information on their previous movements and interactions. A mixed-methods study with key informant interviews from the EVD outbreak in West Africa found that effective contact tracing was restricted due to a lack of community trust and concealing of exposure information. Public trust in the UK COVID-19 test and trace system is variable and challenged by concerns about data security, confidentiality, and a lack of public consultation and input. Qualitative research in ethnic minority groups suggests that they are more likely to participate if the effort has been promoted, endorsed, and reinforced by trusted community leaders, and if the messages are empowering and engender a sense of agency and self-determination. Effective government-citizen cooperation, communication, and public education have been at the core of the aggressive and successful contact tracing efforts seen thus far in Vietnam. Coordinated efforts must involve local authorities, businesses, voluntary organizations, and faith leaders to educate and engage citizens, in turn increasing the impact of TTI systems.
Isolate
Those cases and/or contacts identified as requiring isolation must be in an environment where it is incentivised. Some of the largest local outbreaks in high-income countries have been associated with meat-packing factories where employees did not promptly isolate, due to the risk of losing money or their job altogether. Given the size of the manufacturing industry in MICs, the dearth of pay protection, and the economic pressure to keep businesses open, outbreaks in workplaces are a serious concern. Legislation to protect against this has emerged in some countries, including Brazil, where federal provisional measures, including Provisional Measures (MPs) 936 and 927 have been instituted to socialize the idea that employers may seek to reduce employees’ pay in exchange for greater job security. MP-936 allows salary and hours reductions for up to a 90-day period as well as the suspension of employment agreements (e.g., furlough) for a period of up to 60 days. MP-927 authorizes the use of unused paid leave and holidays still being accrued. India has enacted even stricter legislation through the Disaster Management Act (2005). Orders prohibit employers from terminating employees during lockdown or reducing their wages. But with India only committing $22 billion, or less than 1 percent of its GDP, to its COVID-19 relief fund, it is unclear whether small and medium-sized businesses will have the support they need to meet these new requirements.
Aside from conditions at work, those at home can also fuel the spread of COVID-19. On average, households in low- and middle-income countries are larger than in high-income countries and more multigenerational, with “joint families” being the norm in some countries. Poverty is also an important driver of disease transmission, and MICs house the majority of world’s poor: often in densely populated urban and peri-urban slums. Dharavi, a sprawling slum in the heart of Mumbai, contains 650,000 people spread over just 2.5 square kilometres, with 8 to 10 people living together in tiny 100 square-foot dwellings. Despite the first case occurring in April, only 80 deaths occurred by the end of June. In large part this was thanks to an aggressive test and trace strategy, supported by community isolation facilities for those testing positive and close contacts (over 10,000 people) as well as humanitarian support through free food rations. Institution-based isolation (rather than household) was a fundamental aspect of the success observed in both Dharavi and China. A recent modelling study published in the Lancet found that home-based isolation causes an 8-day delay in the epidemic peak (and a reduction of 7,100 cases), whereas institution-based isolation leads to an 18-day delay in the epidemic peak (and a reduction of 18,900 cases). With a high number of vulnerable individuals in MICs who lack the resources to isolate safely, repurposing existing community facilities, as seen in Hong Kong, will help limit disease transmission. The immediate provision of housing, food, and medicines to large numbers will be a huge challenge in MICs. But for a well-functioning TTI system that is tailored to and supported by local communities, this could prove essential.
Conclusion
As COVID-19 shifts to MICs, test, trace and isolate (TTI) systems of the type seen in high-income countries are proliferating. With the large, dense, young, mobile, poor, and unequal populations residing in MICs, TTI cannot serve as a panacea for disease control, and will be heavily reliant on concurrent public health interventions. The impact of TTI will be especially limited during the peak of an epidemic. Given the opportunity costs associated with investing in a disease-specific service, new TTI systems will need to pursue unified objectives to progress public health beyond COVID-19 alone. They must be deployed alongside targeted investment in health system strengthening, emergency preparedness, disease surveillance, and public health education, aiming to minimise regional disparities in effectiveness. Optimising the TTI system itself will require rationing tests when required (through the consideration of pooled testing during periods of low COVID-19 prevalence and syndromic surveillance during periods of high prevalence), addressing financial and social barriers to testing, investing in community health workers to perform manual contact tracing supported by community engagement, as well as provisions for the vulnerable to isolate safely and effectively.
MICs face a host of common challenges in the design and implementation of TTI systems. If policymakers ensure that these systems are designed and implemented to be sensitive to the local context, they will add value in the response to COVID-19 as well as the future of public health in MICs.
Rights & Permissions
You may use and disseminate CGD’s publications under these conditions.