Recommended
Community health workers (CHWs) are often the first point of care for vulnerable and underserved populations in low- and middle-income countries.
Personal protective equipment (PPE) is required for CHWs to safely support COVID-19 response efforts and maintain essential services. Unfortunately, the COVID-19 outbreak has caused a surge in demand for—and corresponding global shortage of—PPE. While this deficit affects all health workers, recent evidence suggests CHWs in low- and middle-income countries have been disproportionally affected due, in large part, to their incomplete integration within national health systems (Ballard & Westgate, 2020).
CHWs played a vital role in the 2014-2016 Ebola response and are already doing the same during COVID-19: in many low and middle income countries, CHWs are at the frontlines preventing, detecting, and responding to the outbreak (Wiah et al., 2020). CHWs are a significant pillar of basic public health interventions as they conduct contract tracing and support isolation; robust networks of CHWs may be one of the many reasons why some countries (e.g., Ghana, South Africa) have been successfully mitigating spread (Moore, 2020). CHWs are also critical to ensuring that the coverage of essential services does not decline—a common occurrence during crises which can ultimately kill more people than the epidemic itself. Without PPE, however, community health workers can neither stop COVID-19 nor provide health services. (See Box 1 for a discussion of the critical role of CHWs where other health services are scarce.)
Although the UNICEF/WHO/IFRC guidance for community care recommends PPE for CHWs, global PPE shortages and exorbitant price increases are negatively impacting access to the 14 PPE items prioritized in the WHO Essential Supplies Forecasting tool (“Community based health care,” 2020; “Shortage of personal protective equipment,” 2020; Zimmet et al., 2020). At the time of writing, most sub-Saharan African countries seem to have not prioritized CHWs in their PPE allocation in order to ensure sufficient PPE for other key providers. Consequently, some CHWs are given the option to stay home or else do their job unprotected, putting themselves, their families, and their communities at risk (“India coronavirus,” 2020).
Box 1. Why do CHWs matter now?
The term “community health worker” covers a variety of health worker cadres and programs. Generally, CHWs are lay individuals with some training who provide health services in their communities (Olanarin et al., 2017). According to official data from the World Bank on CHWs, there are 3.5 Million CHWs worldwide (Community health workers, n.d.).
CHWs have been critical in places with severe health workforce shortages and where CHWs are often the most accessible point of care (e.g., Malawi, CHW outweigh physicians 33:1 and 95:1 in Sierra Leone) (Community health workers, n.d.). Several recent studies demonstrate that CHWs have been proven to be cost-effective particularly in improving newborn and child health morbidity and mortality in comparison to facility-based care exclusively or other forms of usual care excluding CHWs (Bhutta et al., 2013; Darmstadt et al., 2005; Nkonki et al., 2017). For example, in Mali, the CHW program substantially improved health outcomes over time at a cost of approximately US$8 per beneficiary per year (CHWs were paid a salary) (Johnson et al., 2018).
Moreover, CHWs offer significant long-term return on investment, up to 10:1, fueled by increased productivity from a healthier population, avoidance of future global health crises, and increased employment (Dahn et al., 2015).
The growing focus on the potential of CHWs to help achieve universal health coverage is motivated by substantial evidence demonstrating their effectiveness in delivering a range of preventive, promotive, and curative services (Cometto et al., 2018).
Unfortunately, efforts to protect CHWs are complicated by the fact that CHW cadres are not well-defined: most Ministries of Health lack updated rosters with information on active CHW cadres. The limited standard enforcement and tracking of these cadres suggests that the official reported CHW numbers are gross underestimates, to the point where they have been deemed the “invisible cadre” within health systems (Meltzer, n.d.).
The absence of a publicly available baseline for consolidated PPE needs for CHWs in low-income countries inhibits efforts to protect and equip CHWs during this crisis. We provide a starting point for the magnitude of needs across 24 countries in sub-Saharan Africa that actively rely on a CHW cadre. To quantify PPE for CHWs, a rapid literature review was conducted to assess the number of full-time and part-time across CHWs in this cohort. Evidence-based assumptions regarding CHW workflow and PPE use were used to calculate the annual PPE needs for CHWs. These figures were then validated by in-country field practitioners, either directly from Ministries of Health or implementing partners. The resulting estimates of PPE for CHWs across SSA offer a baseline magnitude of needs that governments, partners and donors can reference for supply planning.
What PPE do CHWs need, and how much?
Many routine care delivery services provided by CHWs risk bringing CHWs into contact with body fluids and require the use of basic protective equipment. The 2010 WHO training manual for malaria RDTs mandates the use of gloves and WHO/UNICEF issued joint guidance in 2014 on the importance of gloves and other protective equipment for CHWs during the Ebola outbreak (“How to use a rapid diagnostic test,” 2009; UNICEF & WHO, 2014). The recent UNICEF/WHO/IFRC guidance for community care (2020) during COVID-19 advises a basic package of PPE required to protect CHWs to ensure continuity in essential service provision:
-
Surgical masks (disposable)
-
Eye protection (goggles or face shields, would depend on the country)
-
Gloves (disposable)
-
Gowns (reusable)
-
Disposable bags (or other container to safely store and discard contaminated items)
Although existing guidance advises the use of different PPE[2] depending on a patient’s classification as a suspected COVID19 case, we assumed that this basic kit would suffice.
For the purposes of this exercise, given the reliance on CHWs to support the continuity of essential care (and greater reliance on them for COVID19-specific efforts such as contact tracing), we conservatively assume that this basic kit would be required annually for the foreseeable future. Supply planning for product deployment will inevitably need to be adapted to local contexts, accounting for transmission dynamics and operational feasibility (i.e., available supply)—both of which will evolve over time.
Findings in numbers:
-
24 countries make up 80 percent of the population in SSA: Angola, Benin, Burkina Faso, Cote d’Ivoire, DRC, Ethiopia, Ghana, Kenya, Lesotho, Liberia, Niger, Nigeria, Madagascar, Mali, Malawi, Mozambique, Rwanda, Senegal, Sierra Leone, Uganda, Tanzania, Togo, Zambia, Zimbabwe
-
These countries rely on 916,000 active CHWs (14 percent are salaried/86 percent are volunteers with some or no compensation)
-
They serve over 400 million people or approximately 40 percent of the African continent
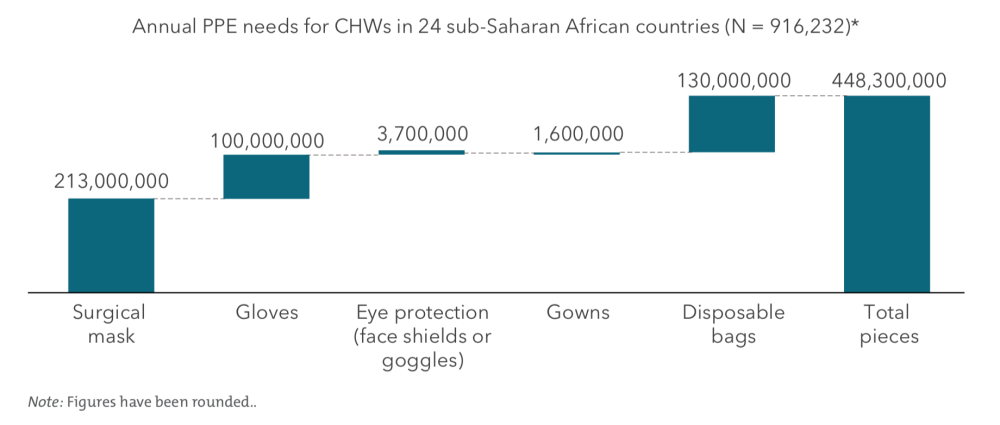
We estimate that approximately 448 million pieces of PPE are required annually (see appendix for full methodology):
-
213 million surgical masks
-
100 million pairs of gloves
-
3.7 million face shields (or goggles)
-
1.6 million reusable gowns, and
-
130 million disposable biohazard bags
Figure 1. How much PPE do CHWs need?
Price of PPE is dynamic and some countries in SSA have started to procure items locally. Based on available unit cost data, we estimate that a minimum of $100M is required each year to meet the above PPE needs. This estimate excludes last mile distribution costs.
This quantification provides a baseline magnitude for annual CHW PPE needs in 24 countries across Sub-Saharan Africa that rely on CHWs. Supply planning efforts would need to account for the following considerations:
-
Current and upcoming stock levels: These estimates do not account for current PPE stock on hand, in transit or planned for as this data was not readily available. Many large multilateral institutions provide funding for at least half a dozen services that rely on CHWs (malaria, TB, HIV, maternal, newborn, iCCM, immunization campaigns) indicating that there may be existing resources funding basic PPE in some community settings. Some funders have supported countries to reprogram a proportion of funds in response to the COVID19 outbreak. With greater attention to the risks of a reduction in routine services by major donors, such as GFF, countries are actively reviewing needs based on existing (and new) resources (“GFF leaders,” 2020). Given that most PPE has 3-5 year shelf life, the risks of over-stocking in the near term are low.
-
The diversity of CHW roles and responsibilities: CHWs may be responsible for at least a dozen different types of preventive, promotional and curative services depending on the country and local context. This analysis at best provides a minimum; countries where CHWs provide a variety of services would require consideration for other PPE items such as N95s and disposable gowns (e.g., TB sputum samples, elderly care, dead body removal, COVID-specific services such as support in isolation wards)
-
Other essential tools: The five basic PPE items in this analysis are proposed as a minimum. Inevitably, CHWs require other tools specific to their contexts including water, sanitation and hygiene (WASH) solutions and thermometers. In addition to supporting routine CHW workflows, digital tools can enable real-time decision-support, community-based surveillance, and contact tracing during COVID-19.
Recommendations for global policy action
Community health worker programs are cost-effective and critical in helping low-income countries, particularly those in SSA, achieve universal health coverage (Lehmann et al., 2019). During the COVID-19 pandemic their contributions become even more urgent. In addition to supporting communities with basic health care, CHWs promote healthy behavior, reinforce public health messaging, and provide social support for their communities. Global health donors and development finance institutions (DFIs) must support community health programs and their supply needs, both during the COVID-19 pandemic and as part of medium-term efforts to build greater resilience in health systems.
-
Ensure PPE needs for CHWs are part of national PPE supply plan: National efforts to procure PPEs for healthcare professionals should not ignore PPE needs for CHWs. Providing PPE in adequate measure for the approximately 1 million CHWs across sub-Saharan Africa (who serve over 400 million people) can cost up to $150M annually. Compared to the scale of financing for COVID-19 ($17 Trillion committed by June 3 2020) this is a relatively small investment (Cornish, 2020).
-
Deploy PPE for CHWs alongside critical supportive interventions: Training, data feedback loops, dedicated supervision and public communications are key for occupational safety and to ensure CHWs are equipped to perform their jobs (Ballard et al., 2018). Health workers have reported encountering stigma from community members who fear health workers are the main source of transmission (Semple, 2020). PPE may contribute to stigma by effectively making it easy to identify health workers. With proper sensitization, communities and healthcare practitioners can harness the protection of PPE to counteract stigma and fear.
-
Investigate opportunities for domestic and regional manufacturing that may serve as optimal sources for basic PPE required for CHWs: Basic PPE items for most CHWs are easier to manufacture as compared to N-95 respirators and other more sophisticated PPE which is typically used for hospital-based care. Domestic and regional manufacturing can arguably offer robust supply of critical PPE for CHWs both in terms of reliability (easier access for stockpiling) and cost. While some small-scale efforts have been started in a few countries, production at scale would require capital investments in existing textile/apparel production lines to guarantee compliance to safety standards and technical/operations expertise to source polypropylene and other fabric used for PPE. Smaller scale manufacturing using manual tailoring can also be a potentially useful source for some forms of PPE. In the case of smaller scale manufacturing, supply aggregation and market connect platforms are required to ensure the output from fragmented production units can be supplied to government purchasing for CHWs. Both types of efforts require additional capital investments, which DFIs can prioritize in their COVID-19 focused investment portfolios.
CHWs serve—and are often from—the most vulnerable and under-resourced communities in the world. Community-level care provision has contributed significantly to the health gains achieved in low- and middle-income countries in the last two decades. However, these gains are fragile and depend upon continuity of community-level care. Delays in getting PPE to frontline workers can reverse these hard-fought public health gains. National governments and global health agencies need to act now to prioritize adequate PPE for community health workers.
Image credit: CDC global.
Acknowledgements
The authors relied on many individuals to iterate, validate, and edit this technical note.
For clinical and quality insights on essential needs and feasibility of PPE deployment for CHWs: Dan Palazuelos (PIH) and Ami Waters (LMH).
We would like to thank the following individuals for their relentless support in finalizing the analysis: Jourdan McGinn, Bailor Barrie, Jennifer Schechter, Kandasi Griffiths, Amutuhaire Maureen, Patrick Zzimula, Lizah Masis, Matthew Ziba, Amy Frost, Michael Erickson, Felix Sayinzoga, Julius Mbeya, Dylan Edwards, Guillaume Mwamba, Craig Usswald, Jennyfer Ambe, Umar Kabo Idris, Likhapha Ntlamelle, Melino Ndayizigiye, Mohit Pramanik, Harriet Napier, Jennifer Foth, Ana Power, Sergio Lopes, Joana de Rosario, Josh Zamor, Emily Bancroft, Jessica Beckerman, Tapiwa Mukwashi, Phyllis Heydt, Temesgen Ayehu, Charles Kambou, Christian Rusangwa, Eliza Walwyn-Jones, Salim Sadruddin, Bradley Didier, Melissa West, Shola Dele-Olowu and Jane Berry.
Rights & Permissions
You may use and disseminate CGD’s publications under these conditions.