Given the massive uncertainty surrounding how COVID-19 will play out in terms of health outcomes as well as economic and social outcomes, policymaking is as hard as it can possibly be. Measures that are sensible at the time they are taken may prove highly costly and ineffective in retrospect. No-regret policies are those that are worth doing now regardless of which scenario actually plays out. This note identifies nine interrelated actions in three areas where developing countries could be proactive: in public health, specifically linked to community health care; in vaccine development, production, and distribution (and other medical supplies essential for the exit and recovery); and in preparing now for a better recovery for economies, firms, and families. Resources spent on these now will not be wasted in any scenario. This note also offers three key lessons for low-regret decisionmaking under extreme uncertainty: collect data now to reduce uncertainty; change and adapt decisions if the data require it; and focus on trust and communication.
There is much debate on what is the right approach to the COVID-19 crisis in developing countries. Should one do a lockdown? Is the cure worse than the disease? And as we all experience now, every week the world seems to be a different place—everyone is forced to learn extremely fast. It is easy then to point to errors in policymaking: no doubt more should have been spent on preparedness, why isn’t there more testing equipment, should a lockdown have been done in the way it was done, did it come too early or too late? The benefit of hindsight is a great tool for criticism.
I have no answer about what the best policy is for tomorrow or next week. This is so unprecedented and there is so little evidence to build on, even from other countries. We don’t know what the end of COVID-19 looks like. Neither China nor South Korea can be sure that they have played out the endgame. Lessons from the past are also poor revision for this test: we can learn something from the 1918 flu pandemic but that was the world of a century ago. Ebola in West Africa is a tempting comparison, but a very different disease. I recall Peter Piot, who was one of those who had identified the Ebola virus a few decades earlier, telling me that it is actually really hard to get Ebola; neither he nor anyone else will say that today about COVID-19. And Ebola did not trigger a global collapse in the economy, even if it was a serious health crisis. Following the science only helps in as far as there is evidence, and there is not much to go on for now, not least for social and economic policies. Before it happened, COVID-19 was one of those famous “unknown unknowns,” and it is only a little bit less unknown now in terms of how it will play out.
In a year or two, many will regret a lot of policy decisions that are being made today. Recriminations will follow. But waiting for better data is not an option: decisions have to be made now as this risks turning into a disaster, not just for health, but also for people’s livelihoods. Rich countries have the option of blanket spending to mitigate this, updating policy as gaps emerge, but in developing countries the resources are just not there to follow this path. No-regret policies should follow the highest priorities: those that are sensible under a wide range of scenarios. No one knows which scenario will play out, but no-regret policies will make sense if current lockdowns work, repressing the virus to a manageable level, but also if the virus spreads fast again and peaks later at even higher levels. They are sound investments if the economic and social consequences are worse than currently anticipated or maybe somewhat better.
I propose nine actions that developing countries and global development agencies can take now that no one will regret later, however this crisis plays out. I offer these actions in three areas: (1) How to save lives as part of the health response; (2) How to make sure we can exit from our current predicament permanently, sooner rather than later; and (3) How to protect the development gains made in recent decades. I do not claim to be the first to argue for some of these, but putting them into a no-regret framework may help to identify other policies too.
1. Saving lives through community health
The viciousness of COVID-19 means that there is no treatment as yet. It kills, and especially the vulnerable, the elderly, and those with preexisting conditions. Even in rich countries, there isn’t that much that hospitals can do, beyond strengthening the body to fight the disease, through oxygen and—for example—nutrition. There are echoes from Ebola in West Africa when some international funders became obsessed with treatment centres and the number of beds they could deliver, while in the end, as Hans Rosling famously said, it was defeated by the already-existing public health teams and their spreadsheets. Getting good data on the outbreak and where it was concentrated, and sending public health teams out to deal with it locally, remains one of the best pieces of advice for now as well as then. Then, it meant community health workers acting as burial teams, with appropriate equipment, and feeding their information back into spreadsheets to track the disease.
We may all agree with the WHO saying “test, test, test” or even “test, trace, isolate” but as long there is a worldwide shortage and predatory buying of diagnostic test kits by some, there is no hope that developing countries can do this at the scale required. However, policymakers can still learn and act now without regret in three health-related areas, and they all involve boosting the support for community health workers and local health centres, and the basic services and information they provide, and not necessarily buying ventilators and the like for hospitals.
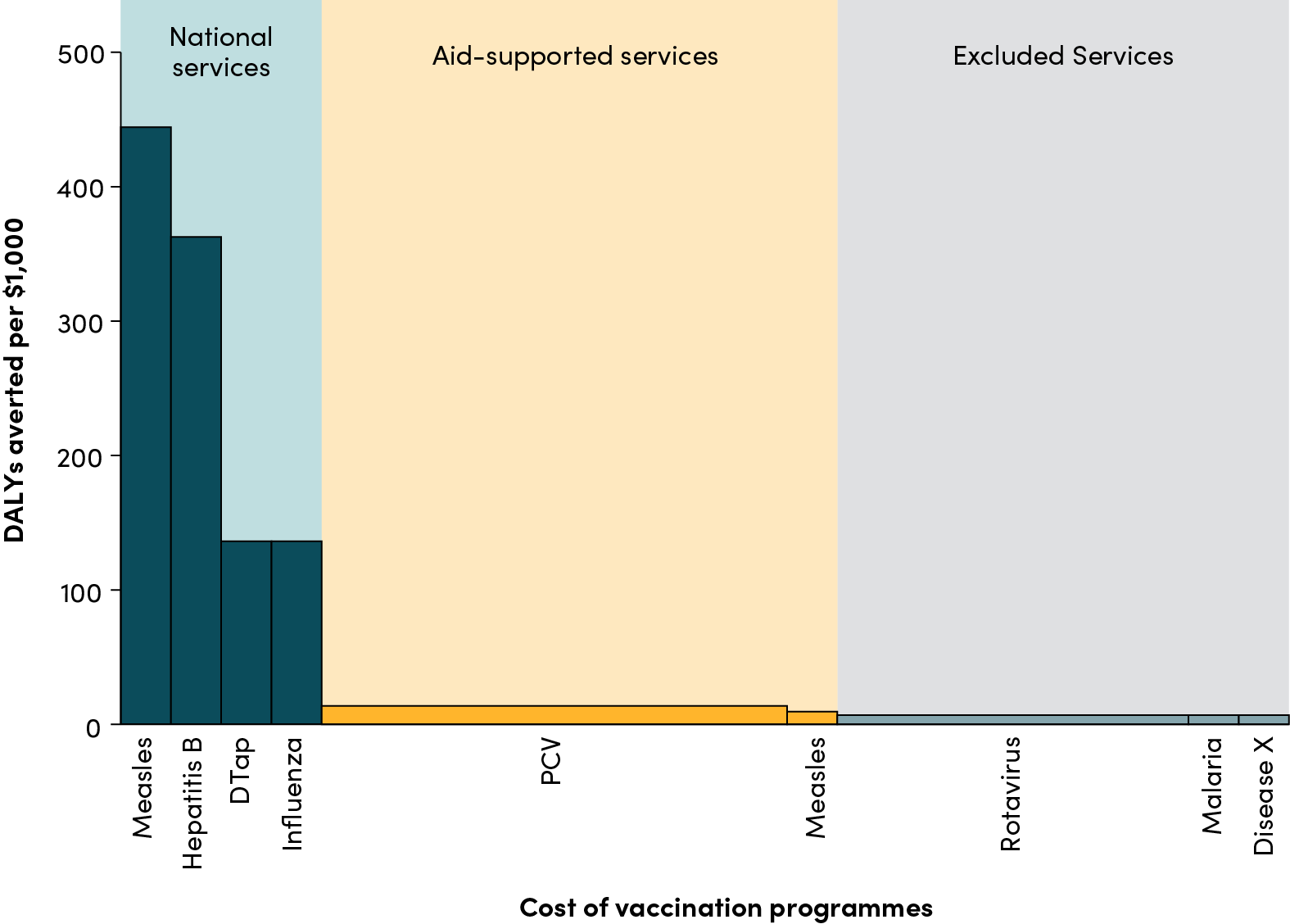
Avoid collateral health damage and make the vulnerable less vulnerable
In rich countries the main argument for lockdowns has been to stop the health system from collapsing, which would risk even more death from other causes. This advice remains valid for developing countries, with one important difference, not least in the poorest countries. Most deaths are averted not through top-end treatment at hospitals but through community health workers vaccinating children; providing postnatal care to mothers; providing supplementary feeding; distributing bed nets; and providing anti-malaria treatment, basic healthcare for the elderly, and more. A huge risk of COVID-19 including from the lockdowns is that these services will stop, making more people vulnerable to other diseases, or maybe even in some cases to the disease we are fighting in the first place. Take vaccinations: they may save about 2 million lives per year according to WHO estimates. Cohorts missed in some parts of the world because of failing health systems for a few weeks would quickly add up to tens of thousands of lives lost. There is no perfect response to this, balancing all the trade-offs with lockdowns. But whatever one does, no one will regret investing in their community health services now.
Concretely, this is the time to make sure these budgets are protected, staff are not withdrawn from these duties and means are explored to make sure they can still reach their usual target population, despite lockdowns, social distancing measures, or other restrictions. It no doubt will also mean investing in basic equipment such as personal protective equipment such as masks and help them with transport to reach all communities. Crowding out of basic health services because of the need to deal with COVID-19 is a big risk. No one will regret avoiding this, even if it costs scarce resources.
Shield vulnerable groups
Even with lockdowns of various forms, uneven enforcement, high population density, and poor water and sanitation will leave those vulnerable to higher mortality rates at great risk. Francesco Checchi from the London School of Hygiene and Tropical Medicine and his co-authors provided some useful reflections on how to shield such populations within families and across neighbourhoods. They suggest a key role for community health workers providing information and advice, in cooperation with community leaders. They focused on the direct health benefits and the contribution to limiting the spread of the disease. Concretely, the role of community health workers in shielding populations can go further.
There are again echoes from Ebola in West Africa, where progress involved public health teams effectively working with communities on behavioural change. Having community health workers and newly recruited volunteers actively reaching communities, encouraging self-isolation, and offering advice on how to limit spread is the first step. If organised well, they can provide an essential link with those in charge of monitoring the spread of the virus. Their reach can also provide a basis of targeted assistance, in terms of food or other essential items.
Investing in water and sanitation or at least ensuring they remain functional now would be another sensible use of resources. Furthermore, a very visible way of containing infectious diseases involves handwashing and temperature checkpoints, familiar to West Africa and the Democratic Republic of Congo throughout the Ebola crisis. COVID-19 is no doubt harder as it involves many asymptomatic cases and pre-disease spells. Nevertheless, handwashing and temperature checks offer a cheap means of hindering the spread or reemergence of the disease.
Test and collate data with the means one has
It is unlikely that large-scale testing will be possible in most poorer developing countries soon, let alone as a means of deciding who can move or not. Testing is just far too limited, as test kits are not available for such countries at any scale. As a result, it appears likely that data on cases are correlated with the number of test kits one has, providing a distorted image. Keeping track of likely cases even without testing was an important part of Hans Rosling’s spreadsheet during the Ebola crisis as well.
The symptom patterns of COVID-19 are increasingly identifiable, and the symptom checklists are widely available. Collecting information based on these checklists—not dissimilar as commonly done for other diseases—will by no means provide accurate information, but still can be systematic, as long as they are done by defined protocols. In any case, they provide better information and are likely to offer more accurate and fast information than what we have at the moment. Getting these spreadsheets will matter this time too; waiting for the perfect diagnostic will be a mistake. Instead, even with imperfect kits, a good system for tracking symptoms, outbreaks, and deaths will help target scarce resources and direct the community health teams to where they are most needed.
It can also help to direct accurate but very scarce diagnostic tests to where they are most useful: testing high-risk populations, or testing community health workers to avoid that they become vectors of transmission. Or to get more accurate aggregate pictures of the scale of the problem through doing random samples of the population.
This would again be something that could be done by an expanded army of community health workers. Investing in community health workers is, however, not just increasing the payroll so more are employed. This matters, but just as in the case of Ebola—which, like COVID-19, is an infectious disease—investing in training and protective equipment for community heath workers will really matter, or they themselves become vectors of transmission. Spending generously on protecting community health workers will save lives.
2. Invest in the exit, especially through vaccines
Every country wants to get out of this crisis. But the nature of COVID-19 is such that even if we flatten the incidence, through lockdowns or other measures, it is unlikely to make the disease go away. The only total exit is a vaccine as it is likely that therapeutics and increased diagnostics will only mitigate its impact. Usually, the entire process of vaccine development takes years, or at least 12 to 18 months in exceptional circumstances. However, in this case, there appears to be a window of opportunity to go faster than ever before by acting now, including through accelerating investment in production and regulatory approval. The race is on, but without global coordination now, development is likely to be slower, poor countries will be priced out this market for a long time to come, and delivery to those most in need will be needlessly delayed. All this requires substantial investment, especially by G7 and G20 countries now, but also extensive coordination with involvement of emerging and developing countries. Below I focus on vaccines, but much what is said is relevant for therapeutics and diagnostics too, and even for quality protective equipment for medical and community health workers. There is an opportunity that ought to be exploited now.
Collaborate on R&D
Many dozens of firms and university research labs are working on a vaccine. A few have just started or are about to start with human trials. CEPI (the Coalition for Epidemic Preparedness Innovations) provides a coordinating role for eight vaccine programmes. Most investment is coming from higher-income countries, some private but also, belatedly, a lot of public money, such as in the US, Germany, and the UK. Vaccines may well become available with variable speed/efficacy/safety features, meaning that the first vaccine, even if we start using it immediately for emergency use, is not necessarily going to be the one we will still be using in a few years. Accordingly, multiple vaccines should be continued to be developed for some time to come. Lurie et al. (2020) explain with far more authority some of the issues and opportunities.
There are obvious ways to push this further, such as by forms of advance market commitments, whereby rewards are linked to speed as well as efficacy or safety features. However, there is an obvious space for collaboration with developing countries too that can help speed up development: with the crisis peaking in different locations at different times, and possible variable seasonality in disease incidence, conducting trials across a variety of geographies in Europe, Asia, the Americas, and Africa will improve the speed at which results from trials can be delivered. If managed well and fairly, this will increase early access opportunities for such collaborating countries, while boosting capabilities. Similar collaboration could be done on doing trials of multiple candidates at the same time, and safety and other regulatory work—stopping avoidable delays later on.
Boost and collaborate on global manufacturing capability
It is highly likely that in the months after a successful vaccine has been developed there will be a huge demand and limited supply. This happened in 2009 with H1N1 influenza. If so, it is easy to predict what will happen: essentially a vaccine war, whereby national interest will be invoked to make sure limited supplies will go to those countries with most purchasing and political power. And as the science is not predictable and it is unclear who will deliver the vaccine at speed with sufficient efficacy and safety, even rich countries may lose out.
There is only one way of avoiding this now: massively pre-committing to the production of as many likely successful vaccines now, by investing in the manufacturing capability and the investment to scale up production rapidly. In that way, supply will be high at the time a vaccine has been approved. This means producing now even before a vaccine has proven its efficacy—and running the risk of having to pour away millions of doses of vaccines. To do so, organisations like CEPI and others could pre-identify some of those that have a sensible balance of speed with likely efficacy, and produce several of them at the same time in vast quantities. Many billions worth of advance market commitments for the production of several vaccines could be issued in coming weeks and months, well before the end of human trials to ensure a vast stock when the trial science catches up.
Would this cost crazy sums? It would be billions of dollars, maybe 10 or more, but given that likely losses to the global economy are already running in the trillions of dollars and even fiscal plans of the G20 are in the trillions, such sums feel like remarkably good value for money.
Development partners can help here, as can other countries with manufacturing capabilities. It is an obvious way for the World Bank Group’s International Finance Corporation to play a crucial role and help identify and spread manufacturing capability for this purpose, also across emerging and developing economies. Massive supply will make shortages and the prospect of a vaccine war less likely, and create the prospect that those who need a vaccine most will get access.
Prepare for delivery of vaccines now via a global deal
Getting vaccines delivered is never an easy task, although it has improved dramatically in developing countries including with support from international organisations such as WHO and GAVI. As long as there are vaccine shortages, the prospect of the developing world— and especially the poorest countries—to lose out is real. No global deal for access to vaccines for these countries in the coming 12 or 24 months is credible unless manufacturing will be boosted at the scale described above. However, even so, the task for delivery will still be huge. It will require funding, it will require much effort—but with a head start, this will be far more likely to be successful. Successful delivery can be planned now through careful dialogue and sufficient funding. Countries themselves can do much of this work; international organisations should get ready to support them on this now; and richer economies in the G7 and G20 should commit and allocate funding now to make this work.
It is true that developing countries are unlikely to be in control in the area of vaccines, as the R&D capability is mainly in the G7 and possibly in China and at most a few G20 countries. However, some others, such as India, may well have the required production or local trial capability and experience to contribute. What is true for vaccines may also be true for therapeutics and diagnostics. The latter will definitely be required for some time to come, as would be protective equipment and clothing for medical staff, and community health workers. For all these there is a window of opportunity to spread their production across firms and geographies, making conflict less likely.
3. Invest now in the recovery, making the crisis more likely V-shaped than L-shaped
Just as for the disease, there is no miracle cure for the economy. No one really knows what needs to be done. The way global economic activity has stopped will make a recession in virtually any country in the world likely. Governments try to balance economic activity with health advice as well as they see fit. In some months only will we begin to learn what would have been the right response.
There are, though, a number of things that can be done now that in any scenario will be useful. The key here is to ensure the recession has as few permanent impacts on the economy as possible, to make sure as few firms and individuals are permanently affected. The aim is to make this crisis V-shaped in the data. The alternative is an L-shaped crisis whereby losses from COVID-19 become permanent in global productivity, and in terms of the incomes and assets of firms and individuals.
As poverty is closely correlated with GDP, for the poor and economically vulnerable in poor countries this is especially risky, leading to some to forecast huge poverty impacts, albeit with a false sense of precision. If these poverty impacts materialize, then the consequences on the poor could also be devasting in other dimensions, such health, that may dwarf the direct mortality impact from COVID-19 itself, as the Center for Global Development suggested. No one can tell with certainty whether the indirect effect of the cure, closing down the global economy, is worse than the disease for the poor, and surely we will begin to learn this soon. However, a number of measures could be taken now without regret to avoid some of the worst longer-term impacts on the economy, lives, and livelihoods in developing countries.
Make sure the poor get cash into their pockets by whatever means possible
Various measures are being taken across the world to make sure that formal sector workers are not laid off and retain some of their earnings. The greatest losers will be those informally employed or self-employed in the informal sector, mainly in the urban centres, but also in the rural areas. There is no perfect response here—even rich economies struggle to provide this support to casual workers and the self-employed. However, the risk is that these vulnerable groups don’t only just lose out now, but also drift into poverty permanently, as they have to sell their productive assets, required for their economic recovery, or cannot sell their produce now so they cannot afford seeds or inputs later, or pay the school fees for their children when schools open again.
To avoid some of the worst impacts on the poor, permanently, it is imperative to provide a buffer now. Any existing systems that provide cash or other transfers should be used to give a further, extra boost, beyond what they usually provide, and expand their coverage if possible, such as to borderline cases or anyone who had graduated out of the system in recent years. Existing systems are widespread, as this econfip brief showed, and they can and should be mobilised.
If there is still a chance to make these transfers via mobile payment systems, it should now be grabbed if it hasn’t already been. Few developing countries, not least the poorest ones, have systems with sufficient coverage. Working with mobile phone providers, it should be possible to offer geographically targeted cash transfer even in contexts where such systems did not exist before. A scheme of this nature is being developed in one East African country by a specialised NGO working with the prime minister’s office. Such schemes could be up and running very quickly, and provide further transfers into areas that are generally poor.
Some governments may be very concerned that there will be leakage to people not requiring these transfers, while it is a fact that mobile phone coverage is not universal among the poor in most countries. No system is perfect, but combining transfers with pro-social messaging (such as encouraging people to pass on transfers they don’t need to the needy) is a behavioural science application worth trying out during the kind of crisis that we’re now experiencing.
Overall, compared to the current cost of the crisis for fiscal budgets, these temporary transfers will save permanently substantial welfare payments and other pressures, and allow many vulnerable people to avoid becoming permanently trapped in poverty once the crisis is over. Instead, it will help many of them to ensure they recover then without further help—an obvious no-regret policy that always will give positive results, even if some may have been able to cope without the support.
Invest in data now to make the recovery sooner and better
Nobody knows how this crisis is really working through the economy. We can observe less traffic, people not going to work, workers losing their jobs, goods not arriving in ports, and more. However, nowhere in the world can we be certain how the economy is being undermined and how resilient it will be once the recovery can start. When it comes to allocating resources for the next month, it is not quite clear where in the economy to spend it best. Nobody knows which parts are most resilient.
There are parallels here with Ebola in West Africa, where the main scenario was one of collapse across the board. I recall ads in Time magazine, sponsored by an international organisation, proclaiming that famine was looming as farmers could not work the land and the next harvest would fail. Careful investment and analysis of food price data and other evidence allowed it to become clear that farmers were not deserting their land, and that an agricultural crisis was not looming across West Africa. It also established that smallholder farmers (constituting the lion’s share of the country’s poor) were not the main economic victims of the crisis, but rather the urban informal sector and rural non-farm workers, dependent on the flow of goods and urban activity in general. It was data that allowed countries and aid agencies to adjust their responses and in this way use resources more effectively, also during the later stages of the crisis and the recovery period.
With COVID-19 (as was the case with Ebola), standard data collection, such as by statistical data agencies, is disrupted. Most of the time, one would typically only trust such sources to guide policymaking. However, these are extraordinary times, and more than ever, the net should be cast more widely. Price data are crucial. Mobile phone data may offer insights in changing economic activity and living standards. More simply, telephone surveys of firms and individuals remain possible and should be used widely, and systematically with clear protocols.
None of these methods are perfect, but if started now, it should be possible to learn quickly, not least how the economic situation is changing and how sectors and geographical areas are affected, to help focus energy and resources to those areas that may require more attention.
Prepare now to adjust later
The global economy will contract and go into recession this year; of that there is little doubt. Recessions are not uncommon and may even play a role in long-term growth. Competition but also business cycles contribute to Schumpeterian creative destruction: the weakest firms may end up disappearing while new firms emerge. Recessions may involve many of the weaker being pushed under, making space for new ones. But this time it is not an ordinary recession. Currently, we see perfectly healthy firms and supply chains being destroyed through the inability to move goods and bring people to work. Assets lie idle or may need to be liquidated, and capital flight from developing countries to perceived safer havens is likely to increase. Central bank response in all economies, however well intended, is creating huge liquidity but not many assets worth investing in. Olivier Blanchard has argued that a huge misallocation of capital is likely in the aftermath, geographically between emerging/developing economies and rich economies.
We need a better way to allocate to support to firms. Picking specific firms to protect will not necessarily target the most dynamic ones, or those whose survival is most important for driving growth during the recovery. Politically connected firms are likely to win the scramble for support. This will contribute to further misallocation of assets within economies—think of utilities that were in dire need for reform, or oligopolistic firms controlling domestic value chains; most countries could easily put names on them. Reforming them during crises is not a good idea; but meanwhile, they will need and haemorrhage more scarce cash.
For many of the poorer or resource-dependent economies, this will spell huge challenges, as debt positions were not strong to start with, and commodity prices and global value chains will take a while to pick up again. They will enter any recovery with more liabilities, both domestic and international, and substantially misallocated domestic assets. This will not lead to a smooth economic recovery, even if it will come with international debt relief and other balance of payments support. Domestic asset misallocation is bound to have become worse, and positions more entrenched; already these countries suffer more from asset misallocation and its negative effects on productivity.
All this means that policymakers in economic and finance ministries and in central banks better be very alert: a messy time will come; it will not be the same as before, like waking up from a bad dream. So what to do? Technocrats will need to think about a country’s balance sheets, and provide support now where it seems needed, but avoid making commitments that are hard to keep later. They should make sure they understand where the economy was weak before, and where it was stronger. It will require careful and cautious management now to make the course-correction later less hard to take. Doing this now will avoid outsiders suggesting conditions from the manual of one-size-fits-all, rather than the best way of handing this within the local economic and political context.
And the technocrats better warn and communicate clearly with politicians now. When Ebola ran its course in West Africa, the then president of Sierra Leone wanted the international community to pay for a project he had long dreamed of: a new airport. There seemed not a thought in his mind then about how it could be paid for, and why international resources should go to that prestige project when the population had suffered so much in the preceding two years. Fortunately, it never happened and at least some resources went elsewhere. Populations across the world will ask and deserve a COVID-19 dividend for the hardship they have endured now. It is crucial not to make that fair request even harder to respond to. People will have to come first.
Some final lessons on policymaking in a world of uncertainty
COVID-19 has no precedent. Its public health and economic impact remains uncertain. It is an unknown unknown: it may be possible to describe some scenarios but by no means all, and one definitely could not attach probabilities to likely outcomes on lives and livelihoods. Even the epidemiological models used to assess impacts depend on a host of assumptions for which data are still not forthcoming. So how can policymaking then be done, if there is so much uncertainty? Three principles will help to avoid regret.
First, as the epidemiologists tell us, data will be key for them to depend less on assumptions and more on evidence. They need better data on population-wide infections over time, so their cry is for more diagnostic data collection. This is a more general point: under uncertainty, the key is to try to lift “the veil of uncertainty” and begin to see what is really happening. Whether in public health or for the economy, the key here is to collect data, and the more data we have the better we can allocate public health resources as well as financial resources to the economy. Given the extreme uncertainty, investing now in data at scale is a clear no-regret policy decision.
Second, by its nature, decisions in this world of huge uncertainty need to be taken based on little or no information. Obviously, it will mean that at times the wrong decisions will be taken. Usually, it is a sign of political toughness never to change one’s mind and make a U-turn; or as Margaret Thatcher famously said, “You turn if you want to, this lady is not for turning.” If ever this was the wrong advice, it is now: in a world of uncertainty, when new data come along, it is crucial to be willing to change one’s mind. John Maynard Keynes’ approach is now more correct than ever: “When the facts change, I change my mind.” Policymaking under uncertainty has to be adaptive: decisions and spending allocations need to be made in ways that can be reversed, fiscally and politically. There should be no regret when decisions have to be reversed when new data emerges.
Third, policymaking under uncertainty, when unknown unknowns rule, is a test for any leader and decisionmaker. Policymaking may seem improvised or based on knee-jerk reactions. This creates problems for any politician, but in the current circumstances even more so: the spread of the virus will strongly depend on individual behaviours based on general public advice. This will only succeed if politicians and government are trusted, and this cannot be taken for granted in many countries, including rich, emerging, and developing countries. Trust is the most valuable commodity, and building and sustaining trust now is key, and will not be regretted. During Ebola outbreaks, trust was central for success. Clear and authoritative communication, explaining in a clear narrative why decisions are taken and maybe reversed, will be essential. Maintaining trust will be the real test of leadership in many developing countries.
Ranil Dissanayake and Kate Orkin provided excellent comments on an earlier version of this note.
Rights & Permissions
You may use and disseminate CGD’s publications under these conditions.