Recommended
Building upon our earlier blog post on COVID-19 and smart health spending in developing countries, we developed a presentation on some of our early thoughts and research findings—focused on current gaps and much needed areas of development in research and resources for better outbreak preparedness.
Here we summarise a few thoughts on important areas for new and sustained investment:
1. Focus on “what works” in LMICs—and at what cost
As many countries gear up response efforts, there is a dire need for evidence-based approaches on what can and will work in different settings with different types of constraints and challenges. There is some limited evidence on effectiveness and cost-effectiveness from past experiences with SARS and pandemic influenza, as well as from current efforts among countries hit early on by COVID-19. Published studies primarily come from higher income countries (HICs) that not only have the resources to address these threats but also the research infrastructure to document experiences. Among studies on COVID-19, as of March 16, only one of 914 COVID-19 studies indexed in PubMed mentioned cost-effectiveness—a laboratory protocol for early detection of the virus coming from South Korean investigators. Some of this information may be transferrable to COVID-19 and adaptable for low- and middle-income (LMIC) settings, but much more will be needed to support strategic allocation of resources throughout ongoing response efforts.
In the immediate term, efforts should be taken to create broader knowledge sharing platforms on how response strategies are conceptualized, what approaches are being taken, which interventions are being used, and the associated resource requirements—all with attention to how such strategies or tools might be adapted in lower-resource settings. These efforts would complement and could build on existing COVID-19 research-focused repositories (e.g., WHO, NIH, Semantic Scholar), and may include an open web portal as a central clearinghouse that shares national and city health response plans, hospital operating procedures for triage, staffing, isolation, and infection control/decontamination (such as those already posted by Public Health England, US CDC, and WHO). It would also be beneficial to have a curated compilation of literature on documented decision frameworks and strategies from past epidemics and disaster responses. Further, researchers should take advantage of the natural experiments occurring within and across countries, using real-time data wherever possible to dynamically inform and update models. These models should include, from the outset, epidemiological and clinical as well as social and economic parameters, all with a view to refine advice and response measures.
It is by now accepted that the fight against COVID-19 will not be a quick one. The disruptions to all affected economies and societies are expected to grow in both scale and scope. As such, beyond knowing what works against COVID-19, we also need to enhance the knowledge base on the inherent tradeoffs and costs of different interventions, policies, and strategies within health and beyond, recognizing that different approaches may be needed in different country contexts based on the fuller range of health and social needs beyond COVID and existing capacities to meet them.
The indirect effects of epidemics on other health services is well documented in the aftermath, but are rarely considered proactively when decisions are made about how to allocate scarce health resources. More work is needed to inform how priority-setting decisions can be made in such a complex, rapidly evolving context including how different epidemic response strategies may negatively impact other key health priorities or disadvantage populations, how serious those consequences may be, and what actions can mitigate these harms.
Integrating such ample evidence in real time is fraught with difficulties, but related streams of work like disaster management have already documented some of them, for example, exploring evacuation practices for vulnerable populations during man-made and natural disasters (e.g., during the 2011 nuclear incident at Fukushima, Japan). The best course of action at the time remains controversial even in hindsight as research findings can be difficult to reconcile. While a number of studies found evacuated nursing home residents actually suffered higher mortality than those who sheltered in place, there is conflicting evidence about the conditions in which evacuation may be preferable, including those related to staff capacity for supporting non-evacuation strategies, conditions of the evacuation site, and baseline characteristics of the population.
While these studies are still too few to be conclusive, they offer valuable lessons and experiences for how to gather evidence and test hypotheses for different approaches, an essential tool if outbreak decision-making is to improve. Similarly, research into adverse effects of different response strategies on other areas like schooling, manufacturing, trade, etc. will provide the broader much needed information for multisectoral epidemic response efforts and optimal approaches given the looming global financial crisis.
Lastly, with more and more LMICs building institutions and processes for evidence-informed priority setting in health (a growing “culture of HTA”), as well as more sophisticated approaches to modelling for infectious disease threats, health policymakers leading response efforts will be much better placed to use evidence to make good decisions in the face of ongoing and future threats.
2. Sustained investments after the event for “lessons learned” and learning healthcare systems
In the mid- and longer-term, more work needs to be done to enable systematic data collection and evaluation of the experiences and impacts of different strategies in various country and epidemic contexts. This would build on the repository of evidence for future outbreaks, including further analysis of: what worked and what did not and why; how decisions were made and what the key gaps decisionmakers faced; and how different preparedness rankings on the Joint Evaluation Exercise or International Health Regulations or the Self Assessment Annual Reporting Tool affected the success or failure of response strategies.
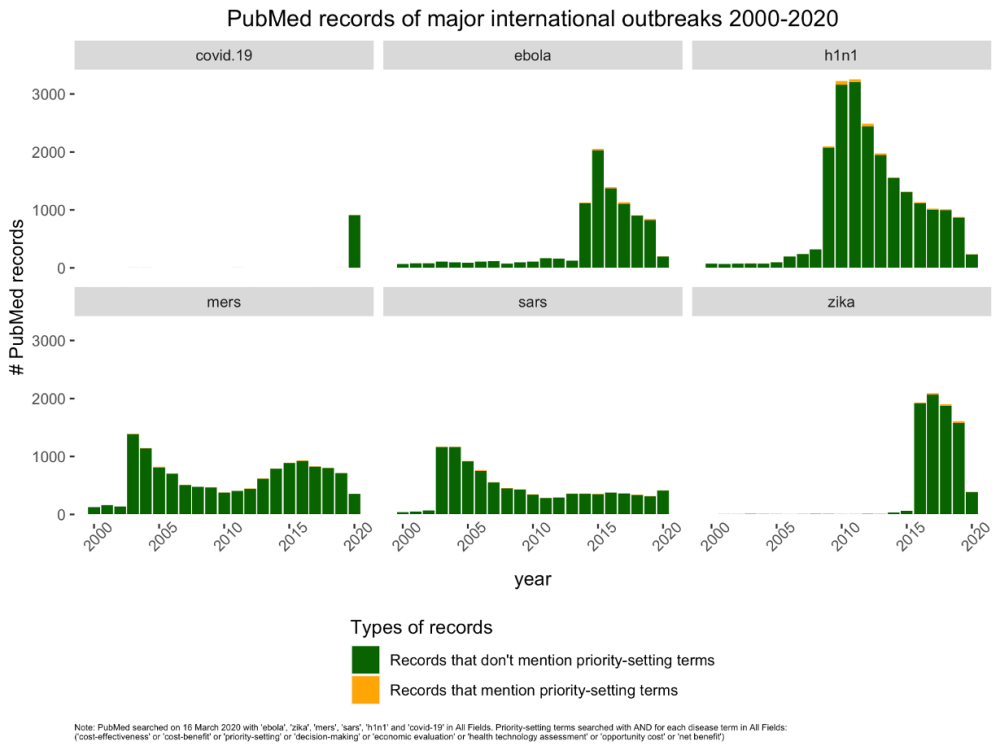
Moreover, this outbreak presents an important opportunity to examine the costs and resources associated with different outbreak response strategies. The amount of research looking into the value and opportunity costs of various interventions is negligible (Figure 1).
Figure 1.
Of 5,537 global health interventions whose cost-effectiveness is recorded in the CEVR Global Health CEA registry, only 11 and 13 refer to “epidemics” and “disease outbreaks,” respectively. (Among the interventions indexed in the GHCEA referred to here, two are from United States. The remaining were evaluated in Uganda, Kenya, South Africa, Pakistan, and Cambodia, among others.) Without understanding the costs associated with different strategies, let alone the potential impacts for those expenditures, it will be difficult for countries and their development partners to advance affordable and sustainable responses best suited to their contexts and available resources.
All of this will require sustained investments in research and in information systems. Clearly, the “boom and bust” funding approach to epidemic-related research has left us ill-equipped to fight future threats with an adequate evidence base. Yet it seems that after the threat of each new epidemic dissipates, funder interest wanes and even existing funds can be diverted to some new emergent threat, as was the case with Ebola monies reallocated to Zika. Our colleague, Amanda Glassman, has already proposed a Global Health Security Challenge Fund to support sustained investments in building preparedness capacity. Similarly, we need lasting investments in research on epidemic threats and response strategies.
Beyond funding for research, we need to invest in the creation of robust research infrastructures in low-resource settings. The ability to assess impacts, costs, and moderating variables (as well as equity of impacts) will be much stronger in areas and countries that have existing ways to capture relevant data points, ideally with “learning health system” approaches. Funders with an interest in the Global Health Security should include “research preparedness” investments to support this type of learning and evidence generation across epidemic cycles. This will also provide much needed information to guide how global health aid should be prioritised in ongoing Global Health Security investments, not to mention the benefits of a learning health system for ongoing Universal Health Coverage goals.
3. Universal Health Coverage is foundational to Global Health Security and must form part of a responsible emergency response
COVID-19 has put a spotlight on how gaps in health insurance pose critical threats to Global Health Security and leave patients vulnerable to both disease and impoverishment. In response to the WHO declaration of a pandemic, Kenya’s private insurers announced earlier this month that they would not be picking up patient bills for COVID-19 related services. Gaps in coverage lead to missed cases and wider community transmission, undermining any early efforts for rapid detection and containment. This underscores the need for ongoing support to LMICs in service of their UHC goals, but also to bolster preparedness for future threats. Much work has been underway to assist countries on the path to UHC, including capacity development for economic evaluation, broader health research activities, and priority setting processes and institutions. Continued support for progress toward UHC and alignment between UHC and GHS efforts can help mutually reinforce these two important global health objectives.
Investing in stronger health systems, research infrastructures, and sustained resources for epidemic research (including R&D, implementation science, and health economics) must form part of a responsible emergency response, and will pay dividends in the face of future epidemic threats.
In support of immediate efforts to foster broader sharing of knowledge, tools, and experiences as they relate to COVID-19 responses, CGD’s International Decision Support Initiative (iDSI) will be hosting, in the coming months, a series of webinars and virtual roundtables to identify key policy questions and available resources as well as case studies of LMIC approaches.
Disclaimer
CGD blog posts reflect the views of the authors, drawing on prior research and experience in their areas of expertise. CGD is a nonpartisan, independent organization and does not take institutional positions.