Recommended

Blog Post
Against the backdrop of universal healthcare coverage (UHC) goals, the rising costs of healthcare delivery, new technologies, and limited budgets, health care payers need to make strategic choices and prioritize those services and interventions that provide the biggest value from money. Health Technology Assessment (HTA) institutions have been created across the globe to help achieve this objective through the establishment of systematic, clear and participatory priority-setting processes. A key prerequisite of successful HTA is good quality data. In this blog, we describe the progress made by India in the past 4 years in developing information systems that are essential to successfully conduct HTA and inform priority-setting decisions. We highlight three initiatives that have improved the availability of information on cost and quality of life in India, identify remaining challenges, and reflect on the key enabling factors that made these possible.
Health Technology Assessment in India
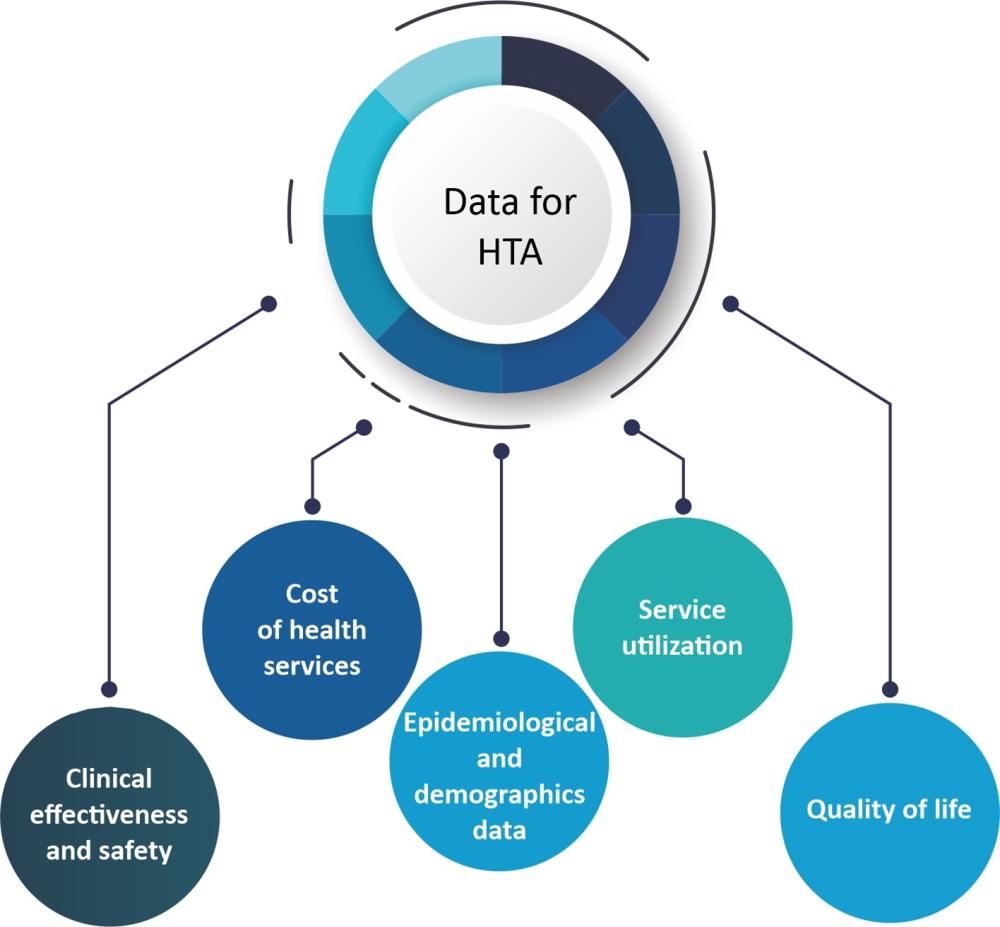
Health Technology Assessment India (HTAIn), the HTA Unit of the Government of India, was established in 2017 to guide health reforms focused on achieving UHC and to assess the implications of investing in new health care technologies or interventions. HTAIn faced challenges in obtaining the high-quality data required for HTA (see Figure 1), and therefore pushed to change the HTA information landscape over the last five years, enabling the generation of locally relevant HTA studies in the process.
Why developing local information systems for HTA is important
Previously, Indian researchers conducting cost effectiveness analysis lacked local data on cost and health-related quality of life (QoL), and were dependent on international resources such as WHO-CHOICE, a disease specific costing resources (HIV, TB, vaccines), or QoL data from Thailand or Britain. Using international resources could be less precise than local estimates due to questions regarding local applicability (i.e., the cost of doing an MRI is different in India than in the UK). With the growing number of HTA studies being conducted in India, it became necessary to develop more uniformity in the data and to ensure validity and comparability of results.
Figure 1: Data requirements for HTA
HTAIn has taken the lead to standardize processes and methods for conducting HTA. This has included developing and publishing the HTAIn “Process Manual and Quality Check Guidelines‘’ which includes the Indian Reference Case for undertaking economic evaluations, guidelines on ‘Budget Impact Analysis’, and the "Handbook on Health System Costing.’’ As part of this effort, HTAIn has also invested in building three critical datasets to provide robust inputs for any assessment conducted in India.
A national health system cost dataset
To answer the question, “how much does it cost?” HTAIn funded PGIMER, Chandigarh, a member of the HTAIn resource hub network, to conduct a nationally representative costing study on 'Cost of health services in India (CHSI)'. The vision was to develop a national reference cost database that achieves transparency along the lines of the UK national reference costs or Australia’s national reference price.
The CHSI study shed light on the cost of services delivered at the secondary and tertiary level of health care, using data collected from more than 75 public and private health care facilities across 11 states in India for selected specialties. These data have informed decisions around health care financing and strategic purchasing, and have been used for revising the reimbursement rates under India’s national health insurance scheme—Ayushman Bharat Pradhan Mantri Jan Arogya Yojana (PM-JAY). The cost data will be accessible on the National Health System Cost Database (NHSCD), a free to use resource, which also provides other useful content such as cost data collection tools, and a tool to predict state level health system costs.
Going forward, a continued effort will be needed to raise awareness of the importance of using local costing data whenever possible and increase the use of the cost database. To match the vision of a national reference cost, the scope also needs to be broadened to include more sites and services and to keep the data up to date. However, cost data collection can be expensive. Mechanisms for regular cost data submission as part of PM-JAY empanelment requirements, could help streamline these efforts and, by involving providers in the process, help validate the cost data generated.
A quality of life tariff value set
To answer the question, “what is the value of the health outcome?”, economic evaluation uses a measure called a quality-adjusted life year (QALY). The QALY is a composite indicator that allows quality and quantity of life to be combined in a single index. Quality of life depends on people's preferences and thus are closely linked to the socio-cultural settings in which they live. To accurately calculate the value of QALYs, the availability of preferences for a representative local population is essential. The Department of Health Research funded PGIMER to lead a collaboration with Euro-Qol Group and other research institutions (Jawaharlal Institute of Postgraduate Medical Education & Research, Puducherry; All India Institute of Medical Sciences, Bhubaneswar, Odisha; Indian Institute of Public Health, Ahmedabad, Gujarat; Academy of Management Studies, Lucknow, Uttar Pradesh) to develop India’s own EQ-5D tariff value set and the first preference-based valuation study undertaken in South Asia. The value set is based on a sample of 3,548 adult respondents selected from 5 states. Recent Indian economic evaluations of vaccinations, technologies, and drugs have now shifted from international values to using the locally generated QoL value set.
While the QoL value set represents an important addition to the data for HTA, the current value set can only be used for generating QoL for those above 15 years of age. However, as 26 percent of the Indian population is under 15-years of age, further work is needed to generate a QoL data set for children.
A database on cancer costs and quality of life
Cancer is one of the leading causes of death in India and access to new treatment technologies are changing rapidly. To facilitate priority-setting in this area, HTAIn is developing a unique open-access, evidence-based resource that will provide information on patient treatment costs, including out-of-pocket expenditure and QoL segregated by cancer site, stage, and treatment approach. As nearly 50 percent of healthcare expenditure is out-of-pocket in India, patient expenditures are an important component of health care costs. India’s database on cancer costs and quality of life currently includes primary data on patient costs and health related QoL, collected from 12,148 cancer patients, recruited at seven leading cancer hospitals across 6 Indian states, and complements the NHSCD that only measures provider costs. The measure of QoL is estimated using the EQ-5D-5L tool and provides QoL values for different cancers segregated by stage and health state. The database has been an invaluable resource for HTA in the area of cancer, facilitating more rapid and less costly HTA analyses, and in turn, helping determine fair prices for cancer specific health benefit packages. But this is the only disease area that has such comprehensive information. The database provides a model for creating standardized QoL and expenditure estimates for other diseases and conditions.
What has made this possible?
The creation of supply-side institutions has created an enabling environment that has led to increased availability of high-quality and standardized information systems for conducting HTA. The government of India's initiative and continued support of the HTAIn has been critical. In turn, HTAIn has supported the implementation of 30 HTA studies, over the last 5 years, and the development of HTA capacity. HTAIn is now at the center of a network of 18 state-level HTA resource hubs across India.
In addition, there has been an increase in demand for HTA from end users such as National and State ministries of Health and Family Welfare. More recently, AB PM-JAY is driving India to develop high-quality data systems for HTA to inform revisions of its health benefit packages for around 500 million citizens that make up the poorest 40 percent of the Indian population. To be financially sustainable, this has created further pressure to generate local cost data as well as economic evaluations to inform health benefit package design.
Conclusion
India has shown how influential government commitment, backed by adequate funding, can help to ensure the development of the infrastructure and information systems to inform HTA. Today, researchers conducting HTA studies in India are able to include various sources of locally generated data.
India's journey highlights that priority-setting institutions like HTAIn need robust data and data systems to support their effective and efficient functioning. However, continued investment is needed to expand the data and make these efforts sustainable. Data must be revised and updated regularly to supply accurate, up to date information that will inform assessments and policy decisions. Getting more health for the money requires robust HTA information systems.
Disclaimer
CGD blog posts reflect the views of the authors, drawing on prior research and experience in their areas of expertise. CGD is a nonpartisan, independent organization and does not take institutional positions.







