With COVID-19 set to lead to a major upsurge in those living in extreme poverty and the wider developing world, the newly released Commitment to Development Index (CDI) provides interesting insight on how 40 of the world’s most powerful countries are contributing on health-related policies and commitments.
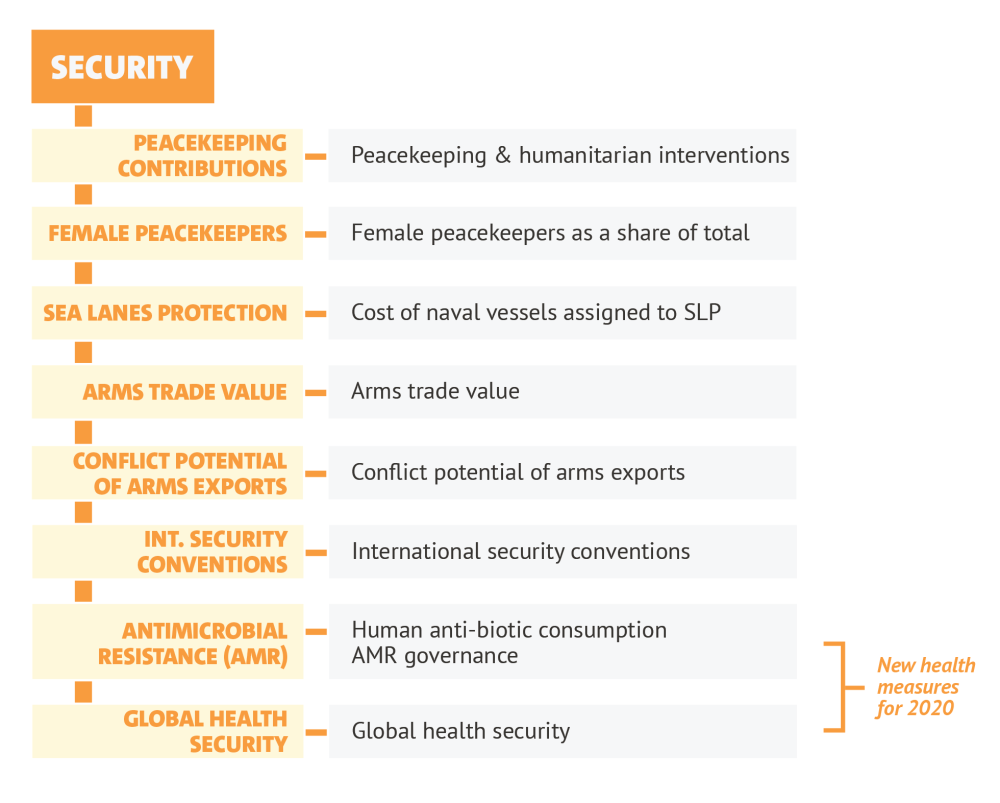
The CDI assesses countries on their policies in seven areas beyond aid that affect development elsewhere: development finance, investment, migration, trade, environment, security, and technology. Health is a new element in the security component, but we also draw out health-related information from development finance, technology, and trade. Specifically, we look at four health-related indicators: global health security, financing for international organisations, research and development, and trade openness.
Sweden, top of the overall index, does well across three of the health-related areas, while the UK and Luxembourg also feature more than once. Still, in trade, EU members’ agreements tend to restrict intellectual property rights with partners, thereby potentially reducing access to medicines. New Zealand, by contrast, does well on its trade openness, as does Mexico, which also uses few antibiotics. South Africa tops the indicator on research collaboration with lower-income partners. The UAE, which ranks last on the overall index, also does well on research collaboration and on supporting international health institutions—showing that even countries with a low overall rank on the CDI can make important contributions to development.
CDI 2020 and Global Health
Today’s CDI launch follows a two-year holistic review of which measures matter most to development. Far before the COVID-19 outbreak, we looked to prioritise global health as an area where countries' policies contribute internationally and “beyond aid.” Consequently, we added new measures on global health to the security component (see image), and we use this blog to draw out the broad analyses on health from the various components of the CDI.
Figure 1. Security component with global health subcomponents
1. Health security: Preparing for the health snowballs and meteors
As the COVID-19 pandemic and ensuing economic fallout have shown, the challenges posed by infectious disease in a globalized world are significant, particularly in lower-income countries with already-strained health systems.
Anti-microbial resistance
In the first new element, we look at the risks posed by antimicrobial resistance (AMR), which is caused by excessive antibiotic use and related pollution (some outsourced). While AMR is perhaps a threat with a slower onset, it is already leading to 50,000 deaths a year in Europe. One study suggests that as many as 58,000 infants died in India in 2013 due to resistance—which will further snowball if no action is taken. The UN warns that drug-resistant diseases could cause 10 million deaths each year by 2050 and inflict damage to the global economy as catastrophic as the 2008-2009 global financial crisis. Our colleague, Charles Kenny, has argued for a global treaty on AMR.
Our measure looks at two aspects of AMR: human antibiotic consumption levels and regulations on antibiotic use, optimisation, and surveillance. Overall, on our measure, the Netherlands, Sweden, and Switzerland score best. In addition, Mexico has the lowest consumption levels. Ideally, we would add a measure for antibiotic consumption in agriculture, but beyond the EU there is no regular international data.
Capabilities for disease prevention
Our second new element measures capabilities for disease prevention using data assembled by the Economist Intelligence Unit and National Threat Institute for the Global Health Security (GHS) Index. It has come in for criticism after it ranked the US and UK top last year, which appeared at odds with those countries’ performance in controlling the COVID-19 pandemic at home. The GHS may not be a good predictor of a government’s performance in managing an outbreak, but it is sensibly constructed, and uses objective and careful assessments of capability.
In any case, our main interest is not domestic performance (though clearly this is relevant in pandemic control)—it is contribution to global capability. With this in mind, we use a subset of measures:
- prevention (including zoonotic disease, biosecurity, and oversight of dual use research)
- detection (including lab capacity and reporting)
- response (including response planning and risk communication)
- adherence to global health norms (including with the WHO’s International Health Regulations, and conducting a Joint External Evaluation).
Across these measures, the United States, United Kingdom, and Australia score well, while Luxembourg and China have the most room for improvement. It seems reasonable that the US and UK are strong on prevention, and especially the human-animal (zoonotic) interface. Still, it’s clear from COVID that capability is only one part of the story, and we’ll consider the continued relevance of this indicator.
2. Financing collective global health
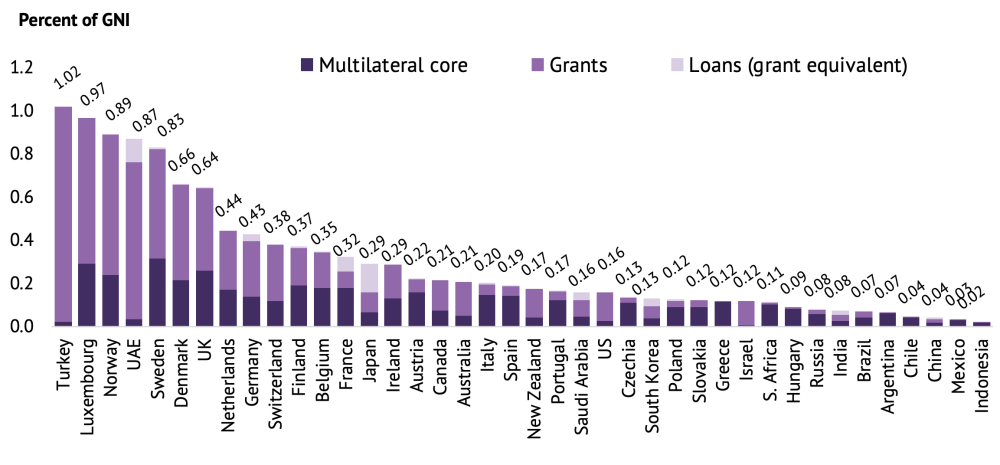
Financial flows to global health are included in our development finance component. Whilst we don’t give particular credit for health (as compared to say, education, climate, or economic development), countries are rewarded for providing financial contributions to multilateral institutions, and in particular towards their “core” costs which have been important in the fight against COVID-19. Such funding enables coordination, economies of scale, and flexibility in responding to new challenges.
Figure 2. Finance for core costs of multilateral institutions
Source: Finance for International Development, 2017
This shows that Sweden leads, with Luxembourg and the UK also giving over a quarter of 1 percent of GNI to multilaterals.
Unfortunately, there isn’t data on all 40 CDI countries that would allow us to examine how much of their overall development finance is focused on health. A very limited indication is provided in the table below showing the top five donors who channel funds to and through three major health multilaterals—WHO, GAVI, and the Global Fund—in 2017 (the year we analyse to ensure comparability across all CDI countries). The largest donors in absolute terms were the US ($1.3bn), the UK ($0.9bn), Germany($0.5bn), France ($0.4bn), and Japan ($0.3bn). Still, to ensure comparability, we use estimates relative to economy size (below).
Table 1. Top 5 commitments to selected health multilaterals, 2017
(share of national income, GNI)
| 1 | Norway | 0.067% |
| 2 | United Kingdom | 0.034% |
| 3 | Luxembourg | 0.034% |
| 4 | Sweden | 0.030% |
| 5 | UAE | 0.023% |
Source: Authors calcs, The Global Fund 2017 Annual Financial Report, GAVI Receipts , UN CEB Financial Statistics
3. Health and technology: Innovations and research partnerships
Perhaps one of the most important ways in which countries can contribute to global health is through developing new technologies: a prominent example is the evidence for the direct role of knowledge and technology in dramatically reducing child mortality.
As in past editions of the CDI, we measure government budget allocations to R&D—as with development finance, we do not privilege any one sector, but a substantial portion will be health-related R&D. South Korea, Austria, and Sweden top the ranking. Research into basic health and neglected diseases is immediately and directly relevant to global development. However, there are other innovations that also have an effect, as new technologies drive the prices of lifesaving technologies down and become more accessible to consumers worldwide (see the full technology component here).
In a new technology measure, we highlight the share of international research collaborations of each CDI country with researchers from poorer countries—many of these collaborations will also be health-related. Building and maintaining equitable research partnerships can help ensure that health research outcomes are mutually beneficial and more likely to achieve the desired development impacts. South Africa comes top on this indicator, with Saudi Arabia, UAE, Indonesia, and Luxembourg completing the top five.
4. Trade: Access to medicines and the TRIPS Agreement
A central problem in global health is reasonable access to medicines, where intellectual property rights play a role. In recognition of these barriers, the WTO Agreement on Trade-Related Aspects of International Property Rights (TRIPS) includes a number of flexibilities for developing countries. However, countries can re-introduce restrictions in their own free trade agreements with developing country partners, thereby eroding this policy space for development.
Here we look at a subset of health-related measures in trade agreements within our intellectual property rights measure from CIECODE. They assess patent term lengths which go beyond the 20-year protection provided by TRIPS (a sufficiently long period of time to enable an innovator company to profit from its invention and recuperate investment costs). They also consider limits on compulsory licensing, a public health tool whereby a government can temporarily override a patent in the public interest to authorize the production of cheap generic versions. Lastly, they consider expansive definitions of counterfeits, which can create new barriers to the production of and trade in quality generic medicines, which are a lifeline for millions of patients in poor countries.
Across these three trade-related aspects that matter most for access to medicines, New Zealand’s trade agreements lead the way, adhering more closely to the flexibilities offered by TRIPS. Meanwhile, EU countries score poorly, as they introduce additional restrictions in their trade agreements with developing countries.
Some countries even improve on TRIPS. Mexico, whose free trade agreement with the Central American Common Market countries (Guatemala, El Salvador, Honduras, Nicaragua and Costa Rica) includes the language of the Doha Declaration, allows countries to export generic drugs produced under compulsory licences to countries which lack manufacturing capacity—including all least developed countries.
In trade, we also look at tariff levels and peaks, especially those against lower-income exporters. Whilst there is clearly unhelpful protectionism arising from COVID, this won’t feed into the data for some time, so we’ll return to that in future CDIs.
Beyond CDI 2020
The goal of the CDI is to inform debates on what constitutes good development policy and to encourage improvements. We welcome suggestions for how to better measure countries’ commitment to global health in future editions of the CDI.
Whilst focus is rightly on coping with the current pandemic, these policy commitments make a fundamental difference to the world’s underlying disease preparedness and health; and the CDI recognises countries efforts in relevant areas.
Disclaimer
CGD blog posts reflect the views of the authors, drawing on prior research and experience in their areas of expertise. CGD is a nonpartisan, independent organization and does not take institutional positions.