Imagine a world in which children in Zambia, Bolivia, and Laos have the same chance to survive, grow, and thrive as their peers in Canada or Europe. Such a world sounds nice, to be sure, but probably quite far out of reach. Yet according to the Lancet Commission on Investing in Health, that “grand convergence” between poor and rich countries is achievable within our lifetimes. This is a remarkable and unique opportunity, one unprecedented in human history.
But what will it take to get there? Last week, CGD welcomed the Commission’s two lead authors — Lawrence H. Summers (also the chair of CGD’s Board of Directors) and Dean Jamison — to share their thoughts on the future of health investments for convergence, based in part on their recent paper in The Lancet. Here are my three big takeaways from their remarks, with major implications for the world’s global health funders.
Middle-income countries can pay their own way … if there’s political will
According to the Lancet report, global convergence will cost $70 billion per year. The price tag certainly sounds hefty — and it far exceeds current aid flows for health. But 70 percent of the global disease burden is now concentrated in rapidly growing middle-income countries (MICs) like China, India, and Nigeria. According to Summers, those MICs should be able to up their health investments with relative ease — if their leaders are willing to take on existing inefficient patterns of taxation and spending. Where to start? Summers suggests hiking taxes on “bads” like tobacco, alcohol, sugar, and extractive industries, plus redirecting fossil fuel subsidies toward the health sector. These policies would be win-wins for health, helping finance a stronger health sector while also dissuading risky behavior. (Like, for example, Thailand’s successful campaign for tobacco control, which will be featured in our forthcoming new edition of Millions Saved).
For the future of health aid, viva la evolution!
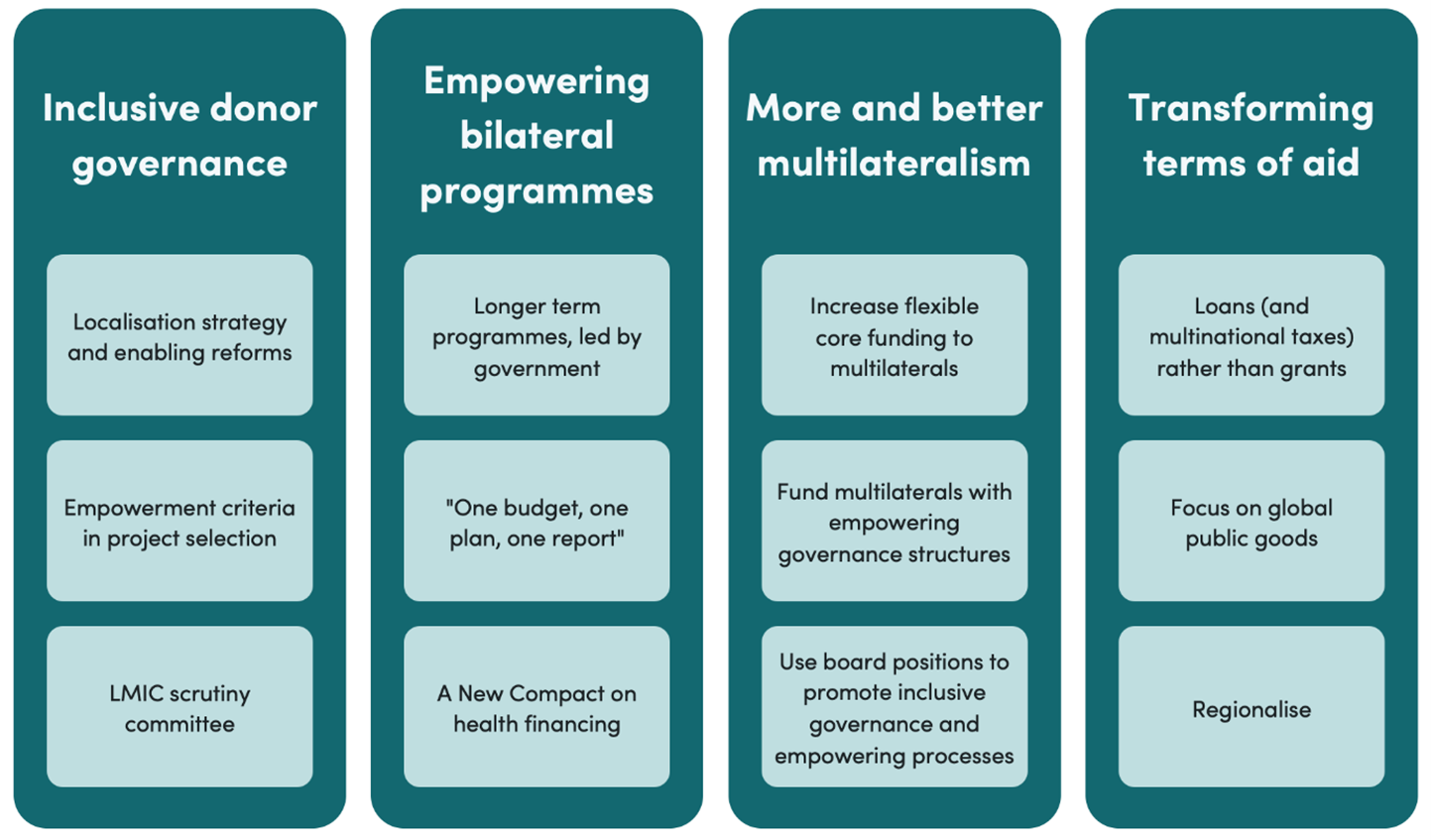
The rise of MICs does not mean the end of health aid; rather, it implies an evolving role for donor investments to achieve convergence. Drawing on their paper, Summers and Jamison suggest a conceptual distinction between two types of health aid. The first type is country-specific — that is, direct support to low- and middle-income countries, benefitting only the specific recipient countries. In contrast, the second type serves “global” functions, including global public goods like R&D, data, pandemic preparedness, and containment of anti-microbial resistance, some of which fall outside the traditional boundaries of overseas development assistance (ODA). With MICs increasingly funding their own health sectors, Summers and Jamison argue that donors should shift their investments toward the latter category, limiting their country-specific investments to the very poorest countries that need external funds to deliver essential services.
The next global fund should fund global functions (repeat 5x fast!)
According to their new paper, roughly four in five aid dollars go to country-specific functions, potentially leaving essential global functions neglected and vulnerable. (For example, Jamison noted the WHO’s lackluster response to Ebola came after many years of sustained budget cuts). To increase those investments, Summers recommended the creation of a new global fund focused exclusively on global goods. Politicians love new and shiny objects, so a new institution might be what’s needed to build momentum for change.
The global health community has an enormous opportunity to capitalize on an historic moment. I hope global health donors will take on this sound advice and make savvy decisions about the allocation of their scarce resources.
CGD blog posts reflect the views of the authors, drawing on prior research and experience in their areas of expertise.
CGD is a nonpartisan, independent organization and does not take institutional positions.