Recommended
Executive summary
Hailed as one of the largest publicly funded health insurance programs in the world, India’s “Modicare” has, since its launch a little more than six months ago, made universal healthcare coverage an election theme for the first time in the country’s history.[1] In this note, we describe the program, with an emphasis on its better-known secondary and tertiary care component, and offer policy recommendations to strengthen the scheme post-election to enhance its contribution to India’s vision for universal health coverage (UHC). In a country of almost 1.4 billion people that is home to one-third of global maternal deaths, where public spending for health accounts for roughly 1 percent of GDP and where 60 million people fall into poverty every year because of healthcare bills, fixing healthcare is a daunting task that will determine the world’s performance against the Sustainable Development Goals over the coming decade.
Healthcare becomes a national priority in India: The origins of “Modicare”
India is a federal country where health is a state subject and government has driven almost all its spending through public entities on the supply side of the health sector since independence in 1947. Over the past decade, however, in response to stubbornly high levels of inequity and ill-health, the central government launched several demand-side initiatives with the aim of improving health and healthcare access for the poor.
The largest centrally funded supply-side program, the National Rural Health Mission, was launched in 2005 and focused on strengthening public healthcare facilities in rural areas by providing additional and flexible funds to state governments. A companion initiative, the National Urban Health Mission, was launched in support of urban areas, and in 2014, both were combined into the National Health Mission, based at the Ministry of Health and Family Welfare (MOHFW). These initiatives played a critical role in public health promotion, perhaps most visibly in the elimination of polio,[2] and in the increase in use of basic health services overall by strengthening public healthcare system.
However, over two-thirds of healthcare services are delivered by mostly unregulated private providers and financed directly by households and individuals out of pocket. Over 70 percent of total spending on health is financed directly by households in India, a worldwide high.[3] Even in public hospitals where care is, in theory, free, data from the National Sample Survey shows that people pay a significant amount (Rs. 6,120, or about USD 90 per episode) out of pocket to receive treatment.
In order to tap into the extensive private sector healthcare delivery system whilst reducing out-of-pocket (OOP) spending, several demand-side initiatives have been tried in India over the years at both central and state levels. Launched in 2008, Rashtriya Swasthya Bima Yojana (RSBY) was one of the most significant centrally funded efforts. RSBY reimbursed public and private hospitals for care provided to eligible below-poverty-line families in an amount up to Rs. 30,000 (USD 4,300) annually. RSBY reached more than 130 million people within five years of its launch, setting the scene for similar health insurance programmes in many states. However, the scheme targeted secondary care conditions alone and many states had in the meantime started their own health insurance schemes, also targeting inpatient care, which continued to run in parallel rather than in coordination with RSBY. In the state of Karnataka, for example, there were eight different public insurance schemes in addition to RSBY as of 2017, each with different eligibility rules for enrolment and different sets of benefits.[4]
Neither RSBY nor any of the state schemes covered primary healthcare and therefore could have had only limited impact on OOP given that the majority (about two-thirds) of OOP on health is related to medicines and diagnostics.[5] On the one hand, many studies to date suggests that neither RSBY nor the state-level schemes[6] nor NHM[7] had a major impact on financial protection, but on the other hand, there are few studies that show that the demand-side health insurance schemes have resulted in some reduction of OOP in both RSBY and state schemes.[8] However, most of these studies also show that access to hospitalisation care has improved because of these schemes. There is a need for the government to have a structured evaluation of both demand-side and supply-side initiatives to systematically analyse their impact on OOP and access. Both supply- and demand-side programs seem to have contributed to strengthening infrastructure and human resources[9] at subnational levels within states.[10]
In part thanks to supply-side initiatives, supported by demand-side initiatives and alongside a period of unprecedented economic growth, India achieved the health MDG goals 4, 5 and 6,[11] and a significant (20-40 percent) reduction in the burden of infectious disease and maternal and child health conditions.[12]
A decade after the launch of RSBY, in early 2018, the government of India announced the Ayushman Bharat program aiming to provide comprehensive cover for primary, secondary, and tertiary care amenable conditions. The program has two pillars that are financed separately. The first is a supply-side investment via MOHFW to establish 150,000 Health and Wellness Centres, supplementing the activities and infrastructure in existing public facilities run by state governments.
The second pillar is a new demand-side initiative, Pradhan Mantri - Jan Arogya Yojana (PM-JAY), that aims to provide insurance coverage for hospital care up to Rs. 500,000 (USD 7,143) per family per year, to about 500 million of the poorest and most vulnerable populations in the country.[13] PM-JAY, which quickly came to be known as “Modicare,” aims to reduce catastrophic out-of-pocket expenditure on hospital bills, improving access to quality health care, and improve health outcomes.
PM-JAY is a targeted scheme initially covering the 107.4 million families (more than 500 million individuals) identified based on deprivation and occupational criteria in rural and urban areas respectively to be poor and vulnerable[14] per Socio Economic Caste Census (SECC) data. The government has announced the scheme may expand to cover more beneficiaries in the future. As it stands, the scheme covers almost all hospitalisation and day surgeries but does not cover outpatient services as they are covered through first pillar Health and Wellness Centres of Ayushman Bharat.
The main focus of PM-JAY is to tackle catastrophic health expenses that push more than 60 million people into poverty every year in India.[15] Many state governments have further expanded PM-JAY to cover more families, consolidating existing schemes funded by the state government. In fact, some states—such as Chhattisgarh, Karnataka, Meghalaya, and Uttarakhand—have already universalised the scheme, while states such as Himachal Pradesh have provided an option to the above-poverty-line population to join the scheme after paying a premium. By our estimates, after expansion led by the states, more than 700 million people are, in principle, covered by PM-JAY and state-funded health insurance/protection schemes.
The states have been provided flexibility to decide on the mode of implementation. Scheme management options include using for-profit insurance companies (“insurance model”) or setting up an independent agency at the state level (“trust model”) or using a combination of both systems (“mixed model”). At present only four states out of 36 states/union territories have not joined the scheme. From those 32 states and union territories that have joined, 17 are using the state-run trust model and the rest are using either private insurance or a mixed model.
PM-JAY is completely tax funded and the cost is shared between federal and state governments in a 60:40 ratio respectively for most of the states and union territories with legislation. For hill states and north-eastern states, the central government bears 90 percent of the total cost, and for union territories without legislation, the government of India pays the entirety of the cost. Beneficiaries are not expected to pay any premium or registration fee under the scheme and are automatically enrolled by virtue of being listed as an “entitled family” as per SECC data.
To manage the program at the national level, the government of India set up the National Health Agency in May 2018, which was converted to National Health Authority (NHA) in January 2019, boosting its status. This quasi-independent body, managed through a governing board chaired by Union Health and Family Welfare Minister, is headed by a full-time chief executive officer (CEO) in the rank of Secretary of Government of India. Even though it is under MoHFW, NHA has been given full responsibility and powers to manage the scheme. NHA is primarily responsible for policy decisions, defining benefits, development of clinical guidelines and norms, providing the IT platform, developing operational standards, processing and analysing claims, and sharing of learning among States. At the state level, State Health Agencies have been set-up as responsible entities for the implementation of the scheme. These agencies have their own teams and receive funding from both central and state budgets for their operations.
India as part of the global UHC movement
India’s move to introduce PM-JAY is part of a broader global movement towards universal health coverage with the aims of expanding financial protection and improving health in countries around the world. Thailand’s UC;[16] Indonesia’s BPJS;[17] China’s recent and less well publicised unification of its urban and rural insurance schemes [18] into one all-powerful Medical Insurance Administration under the country’s State Council;[19] Brazil’s and Mexico’s longer-standing SUS[20] and Seguro Popular,[21] respectively; and South Africa’s blueprint for rolling out National Health Insurance[22] all are examples of emerging economies moving to implement their vision and political commitment to offering access to healthcare services to their populations, oftentimes starting with the poorest and most vulnerable. These models are being emulated by countries around the world striving to implement UHC through a progressive universalism strategy.[23]
The modality chosen by the government of India for implementing the PM-JAY vision provides various implementation options to participating states. As health is a state subject in India and most public spending on health happens at the state level,[24] a “one-size-fits-all” model was a nonstarter. Instead, a great deal of flexibility has been provided to the states in the determination of the exact institutional arrangements put in place to govern and run PM-JAY. States are free to use the IT system provided by NHA or they can use their own existing/new IT system. Additionally, states can use private or public insurance companies as state-level purchasers, directly purchase through government payer agencies, or implement a mixed model. Services are purchased from both public and private hospitals. The model of implementing the scheme at state level aims to align and consolidate existing state health insurance schemes and co-branding has been done between PM-JAY and state schemes.
This approach is not entirely dissimilar to what other middle-income countries have pursued; for example, Colombia uses public subsidies to cover the poor and operates a system of competing public and private insurers which in turn contract with either public or private providers.[25] The health system has managed to drive low baseline insurance coverage and regressive public subsidies in 1993 up to virtually universal coverage with low out-of-pocket spending and better health outcomes in two decades.[26] However, Colombia unifies the finance and purchasing of primary care and hospital benefits in a single insurable package. Similarly, Germany, Israel, and the Netherlands implement a European social insurance model,[27] and are all long standing and well developed systems with a track record of strong performance on equity and effectiveness, coupled with strong regulatory capacities.
Unique features make PM-JAY significant and likely to last
Several features of the design and initial rollout of PM-JAY make its relevance and sustainability quite likely—and argue for increased focus on making PM-JAY work as well as it can for healthcare quality and impact on health under the existing arrangements.
Kicking off an irreversible trend towards universal health insurance: The PM-JAY scheme marks a significant step towards UHC in India. The explicit political backing, ownership by MoHFW, and resulting momentum and speed of implementation is creating a sense of entitlement and a constituency of beneficiaries, especially amongst the poorest, making the policy hard to reverse. Its launch signalled (and perhaps even triggered) a change of heart in the Indian administration on public spending on health. The administration recently again committed to a significant increase in government spending on health to 2.5 percent of GDP, up from historic spending levels of under 1.5 percent GDP,[28] and this commitment is being played out in the national election campaign and across both major parties.[29] Indeed, PM-JAY has made health a top election issue for the first time in India’s history. Now the debate driven by the opposition parties is whether to take an extra step and make healthcare a “right” akin to the right to education and the right to information already in force in India. Furthermore, large-scale state and private sector (insurance companies and healthcare providers) engagement in delivering on the PM-JAY promise is fast creating a multitude of political and commercial constituencies with significant economic interests, which carries benefits but also risks (discussed in the next section).
Enabling a strong pro-poor focus: The scheme is by design pro-poor as it automatically provides entitlement to poor and vulnerable families identified based on Socio Economic Caste Census data. Through state-level implementation, it is already generating positive spillovers, with states consolidating and converging existing state-level insurance schemes reaching richer populations and bringing the total number of beneficiaries to more than 700 million countrywide.
Preventing catastrophic spending and healthcare cost-related impoverishment: PM-JAY in its current form aims to be mainly a financial protection scheme, with the explicit goal of reducing out-of-pocket spending, which in India comprises two-thirds of total healthcare expenditure,[30] disproportionately affects the poorest, and is a major cause of households falling into poverty. Fewer than one in six people in India have any form of healthcare insurance even though about a quarter of all households experience catastrophic healthcare spending during a year. Worryingly, health-related impoverishment seems to be increasing almost twice as fast amongst the poorest compared to richer households, perhaps an undesired consequence of being better able to access healthcare in the first place. Prioritising financial protection is a laudable objective, particularly as evidence suggests that the previous demand-side schemes failed adequately to tackle catastrophic spending.[31], [32]
Openly engaging the private sector: PM-JAY engages the private sector in both commissioning (or paying for) and delivering services. Private providers dominate the Indian market by current utilization and spending, and also in terms of public perceptions of quality and performance (although in reality the public sector may be providing good or in some case even better-quality services as well). Bringing the private sector in as a major implementing partner of a national pro-poor scheme can, if managed well, shift the public’s perceptions by encouraging public providers to up their game while enhancing the efficiency, quality, and accessibility of the private sector for the poorest, through an extensive regulatory empanelment process and efficient rate-setting process already underway. Although more than 7,500 private hospitals are already empanelled under PM-JAY and two-thirds of PM-JAY care episodes are dealt with in the private sector,[33] package rates provided under the scheme are still an area of contention[34] and many bigger hospital chains are holding off joining whilst negotiating higher rates.[35]
Strengthening the public sector: Public hospitals receive the claim payment for treating beneficiaries of PM-JAY directly and enjoy flexibility in how they use this to cover costs incurred. For example, a percentage of the claim could be paid to hospital staff as incentives. This additional money to core government funding, channelled through the demand-side route as a flexible pot that providers can use as they wish, can go a long way in improving the performance of public hospitals, as it can create competition with private providers within the scheme.
Supporting states to consolidate multiple, small-scale coverage initiatives PM-JAY is acting as a catalyst across India, with an increasing number of states enrolling. As of April 2019, 32 out of 36 states have agreed to join the scheme and most have already launched it. States are leveraging the political momentum and additional central-level resources to both consolidate and scale up coverage, resulting in approximately an additional 200 million beneficiaries joining from state schemes. At the same time, PM-JAY is helping to modernize state operations and data and technology infrastructure.
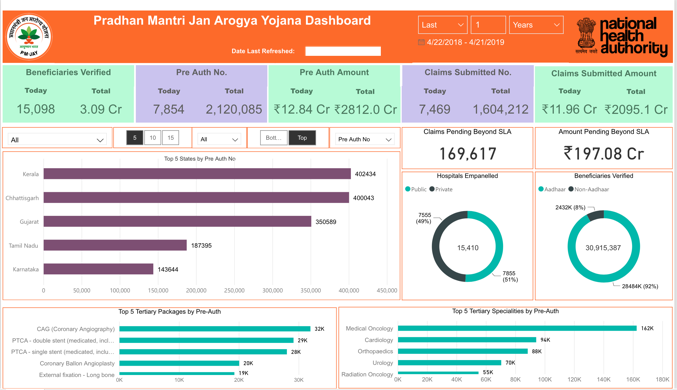
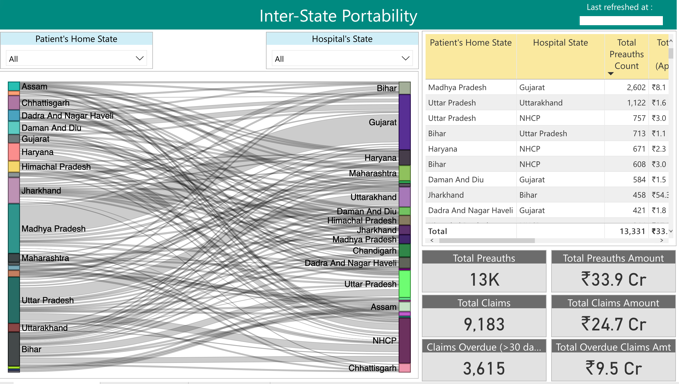
Leveraging India’s technological edge: PM-JAY is both benefiting from and triggering significant technological innovation, including the de novo development of a sophisticated IT system building on and improving existing platforms, such as the Transaction Management System of Telangana. PM-JAY’s IT system allows, amongst other things, online identification of beneficiaries, online software for patient treatment and potential for decision support, real-time tracking of patient flows including across states, and monitoring of outcomes through sophisticated dashboards which can form the basis of electronic registers and clinical audit (electronic dashboard). Another advantage for PM-JAY is availability of the Aadhaar platform for biometrically identifying beneficiaries. The scheme is also developing a strong anti-fraud approach based on data analytics working with reputable developers in the field.[36] PM-JAY has developed real time dashboards to monitor the scheme.
However, challenges remain. For instance, PM-JAY’s IT system is not connected to the various IT systems of MoHFW, which is a priority for producing a seamless integrated IT platform.
Opportunities not to be missed and early warning signs...
While the advantages and staying power of PM-JAY is evident, a number of modifications needed to deliver on the promise of the new insurance program.
In defining benefits, tariffs, and premiums, process matters: Given time pressures and a narrow political window of opportunity, the processes underpinning core design elements of the scheme have not yet benefited from public scrutiny or academic review. For example, there has been, perhaps understandably given the constraints, limited definition of and transparency in processes for designing the PM-JAY benefit packages, or how these were costed, how reimbursement rates were set, and, relatedly, how premium rates were determined. Moving forward, and as all of the above elements of the scheme are likely to have to be revisited, refined, and adjusted, a set of standard operating procedures (SOPs) and guidelines need to be set out determining how (in terms of process and methods) such adjustments are to take place in the future.
There is a clear and pressing need to establish an ongoing process which engages stakeholders, political and technical, in a managed fashion, and which can help inform the tough decisions on what PM-JAY will pay for, for whom, and how. Such a process will also be much more defensible in the public and amongst state and private sector implementing partners, and would make difficult political and technical decisions easier to defend and harder to manipulate by interested parties,[37] and empower NHA and the government of India to keep a tight handle on performance and spending as utilisation predictably shoots up.
PM-JAY has to convince both those worried it crowds out primary care resources and inappropriately favours private industry,[38] and those private sector players complaining it is squeezing their margins too much, making it financially not a viable business proposition.[39]
With adequate evidence and deliberation built into the process, such SOPs can be used to drive both efficiency and quality leading to better outcomes (more on this below) and could include, but not be limited, to:
-
A process for reviewing, adjusting, and updating the benefits, the benefits plan structure, including clinical indications, as well as criteria for inclusions and exclusions, and for appropriate levels of facility and/or quality to offer a given service, as well as upward and downward referral rules including in relation to PHC
-
A guide for best practice for costing benefits and actuarially deriving both utilization estimates and viable premium levels and reimbursement rates, for risk and geography-adjusting contributions and provider payment rates, and for assuring that benefits to be financed are affordable within the fiscal envelope established each year by the Ministry of Finance.
-
A reference case for carrying out economic evaluations of services and technologies, based on international best practice[40] and drawing on the particularities of the Indian healthcare system, to guide Indian institutions such as HTAIn and centres of academic excellence as well as product developers, in submissions demonstrating the value for money of their products.
-
Clear guidelines setting out what the relative roles and responsibilities for designing quality assuring, implementing and monitoring the impact of PM-JAY amongst agencies and levels of government and also research institutes of excellence across the country.
Quality is not an optional extra: PM-JAY is right now—by design—a predominantly financial protection scheme. It will realise its significant potential only when it matures into an effective vehicle for purchasing better health for the nation. Past experience, including with RSBY,[41] shows a significant structural deficit in documenting and promoting quality of care financed through publicly sponsored insurance schemes.
-
Use the benefits package to buy health: Buying health outcomes is a complementary and essential element of UHC. PM-JAY has an opportunity to understand and promote better quality of care by adjusting the way it determines, pays for, and monitors the impact of the benefits it offers to Indians through the PM-JAY benefits packages. Costed Standard Treatment Guidelines (STG) and Health Technology Assessment (HTA), both of which India has invested in over the past few years, are tools for getting evidence of clinical and cost effectiveness into purchasing decisions. HTAIn,[42] under DHR,[43] has tapped into a nationwide network of research institutes to produce its first analyses, including a comparative assessment of intraocular lenses for cataract operations that includes a recommended reimbursement ceiling that can inform NHA benefits listing and procurement.[44] The STGs and clinical flows developed by NHSRC[45] and ICMR as well as the National Cancer Grid[46]—both prepared in a consultative and methodologically robust fashion—are institutional and knowledge assets which can help link payment and volumes to better outcomes and more health for all Indians.[47]
It is heartening to see that NHA has already made efforts to partner with DHR, National Cancer Grid, and others. These efforts will be important for ensuring quality services. The inclusion of clinical indications, referral thresholds, and appropriate sequencing of interventions, as well as defining the setting (secondary, tertiary setting) in which certain interventions can take place, are clear next steps for NHA, as are the introduction of audit and consent requirements as prerequisites for reimbursement for select interventions. All are tools well tested in other systems for linking payment to quality. For example, Chile has AUGE,[48] a detailed list of diagnoses-STG pairs that automatically entitle Chileans to access certain quality- assured services, within a certain time period and within a redefined co-pay, with clinical audit and redress modalities built alongside to enable enforcement.
-
Embrace primary care: Much criticism of PM-JAY has focused on the government’s plan to run PHC through the first pillar of Ayushman Bharat— Health and Wellness Centres—rather than as a part of the benefit package reimbursed by PM-JAY. [49] Critics point out the lack of primary care coverage in PM-JAY[50] and many suggest public monies go to primary care rather than schemes like the PM-JAY that target hospitalisation.[51] However, as the CEO of NHA pointed out, the first, though much less discussed, pillar of Ayushman Bharat is about setting up Health and Wellness Centres to deliver primary care.[52] The challenge remains how effectively to link these two pillars (Health and Wellness Centres and PM-JAY) and existing state-level provision of primary healthcare to ensure a continuum of care and balanced funding to meet the needs of patients and citizens.
To the extent that PM-JAY commits to improving quality and outcomes whilst managing spending, it must consider a proactive partnership with the Indian primary care system, including primary and, most importantly in the shorter-term at least, secondary prevention. These are all central to managing a growing disease burden, especially for non-communicable diseases, and enhancing efficiency of spend. End stage renal disease and access to dialysis are a case in point. A highly cost-effective, inexpensive secondary prevention strategy that combines managing risk factors such as diabetes and hypertension through inexpensive medication, lifestyle changes, and primary care monitoring with routine testing can prevent a catastrophic event (i.e., renal failure). When the partnership between PHC and hospital care is weakened, as in the case of end-stage renal disease, then hospital-driven interventions such as dialysis and transplantation quickly become a major drain on resources with opportunity costs related to spending on other diseases and populations equally worthy of accessing care.[53] Perhaps instead of pitching PHC against PM-JAY, and acknowledging that a strong primary care system alone is not sufficient to deliver on UHC, PM-JAY can lead the way by linking more formally with Health and Wellness Centres as the latter build up[54] as well as seeking opportunities to provide appropriate secondary prevention and management interventions as part of PM-JAY.
For the Chinese Health Minister faced with hospital overcrowding surging tertiary care bills, the solution is obvious: “A successful tiered healthcare delivery system cannot be achieved without a robust primary care system within which GPs are fully empowered as gatekeepers. Additionally, transformation from the current hospital-dominated health-care delivery model to an integrated primary–secondary health-care model is essential.”[55]
-
Leverage technology: Given PM-JAY’s reach, potential for data sourced and analysed and India’s technological industry global edge, PM-JAY can spark the development of innovative Made in India Decision Support solution, which can plug into the NHA claims system as well as DHR/NCG/ICMR norms to can help guide evidence informed prescribing and practice at the bedside and reduce inappropriate care at the insurance level. There is significant academic and commercial interest in such real-time solutions and India in a position both to service its UHC aspirations and the global market.[56]
Assuring value-for-money: PM-JAY’s current emphasis on achieving volumes quickly is understandable given the size of unmet need and urgency. But coupled with a limited handle on quality and expenditure and under-growing private sector pressure, this set-up may fuel overuse and supply-induced demand. The current list of benefits effectively concentrates common reasons for hospital use but fails to convey priorities in terms of quality, value, or outcomes. Better use of resources will enable PM-JAY to cover more services for more people as India realises its UHC vision and adopts the latest technological innovations currently in high-income country systems’ baselines.
-
Use the PM-JAY package (again): In addition to linking payment to quality, the PM-JAY package of services can be used as a vehicle for improving efficiency in delivering care, including through normative reimbursement rate caps for selected bundles of services; disincentivising, through less attractive rates, overuse of technologies and care where there is no clinical indication, including hysterectomies for heavy bleeding, C-sections, proton beam therapy, pacemakers or MRI staging of advanced metastatic cancers; and incentivising good quality indicated services such as vaccinations, early diagnosis and management of cancer, and day case surgery and swift patient mobilisation and discharge post op. On the latter, the current benefits list requires minimum inpatient stays as a prerequisite for reimbursing certain procedures such as stenting, which in the US and EU have much shorter inpatient stays. Using reimbursement rates for clinically inappropriate procedures as a means of risk sharing between NHA and insurers and between insurers and providers can tackle overuse, which is endemic in certain sectors in India,[57] and improve quality whilst containing costs.
-
Take advantage of Health Technology Assessment to buy wisely: India is developing its HTA infrastructure which can drive value-based pricing now (we mention earlier HTAIn’s comparative assessment of Intraocular Lenses for cataract operations which sets a reimbursement ceiling for informing NHA listing and procurement[58]) and signal to product developers the country’s willingness to pay for innovation in the future.[59] There is plenty of precedent for such approaches including from the British National Health Service.[60]
-
Regularly update costings, tariffs, and risk adjust as needed: It will be essential to establish a routine process to collect ongoing data and course correcting benefits packages’ costing exercises allowing for risk, patient mix and geographical, cost of living and transport adjustments. Continuous costing can help inform premium and tariff revisions, improving trust and driving uptake by private providers whilst protecting against wasteful spending and assuring that expenditures—planned and actual—fit within the given fiscal envelope.
A PM-JAY data revolution: invest in routine data and M&E. The PM-JAY generates rich data that can be used for not only improving implementation but also for policy inputs. The scheme’s dashboard can potentially offer a wealth of information to drive strategic purchasing and provider payment reform; inform clinical audit, thereby improving clinical governance and quality; and demonstrate impact on health and on spending. And this is still early days. But for the full potential of the PM-JAY to be realised, the collected domains need to be rethought and a proactive M&E unit set up to articulate targeted need, clean up and analyse the data, and offer its findings in a user-friendly format to NHA and SHA policy makers.
-
Inappropriate use, intentional or not, has similar effects to fraud. However, the highly sophisticated fraud detection mechanisms embedded in PM-JAY are not matched by strong controls for inappropriate, wasteful, and at time harmful, care. Listing and reimbursing by clinical indication and subgroup, and appropriate tiering and sequencing of services, can reduce waste and improve outcomes, as discussed in the quality section above.
-
Routinely collected data offer unique opportunities for course correction Having access to the right kind of data in a timely and user-friendly fashion empowers payers and service users. The kinds of data we are referring to and which are used extensively by many successful UHC systems around the world include but are not limited to e-registers and national and subnational audit and benchmarking (e.g. atlases of geographical variation in access/utilisation, outcomes and spend a lot of it done through OECD for HICs and some MICs[61]) to monitor quality and the use of patient reported outcome measures (PROMs) for routine procedures to identify outliers and adjust reimbursement.[62]
Made in India for UHC: Emerging powers such as China[63] and Brazil[64] have been using their domestic healthcare market to fuel their own healthcare industry. Manufacturers of healthcare commodities, private providers, and private insurers can access an Ayushman Bharat guaranteed market and in return for volumes and revenue they can offer better prices, comply with better regulation, and share their performance data to allow benchmarking and encourage healthy competition.
Streamlining of programs (national, within states, and across diseases)—the end of verticals? We have already discussed the emerging synergies between the PM-JAY and state-level schemes, combining the pool of beneficiaries and producing economies of scale and technological innovation. An additional opportunity for economies of scale and of scope is that of converging the country’s vertical programmes. TB, vaccination, and others (e.g., dialysis and cataract operations)—all are funded centrally through vertical cash flows and separate from the PM-JAY effort. Effective coordination across diseases and technologies can generate efficiencies which the country cannot afford to ignore. However, one important factor to consider here would be that PM-JAY is a targeted scheme while the vertical programmes are mostly for all the population.
Last but not least...procurement: The NHA holds no funds centrally other than grant-in aid to states and their own administrative costs; MOF transfers funds directly to states according to the number of eligible beneficiaries and the co-financing arrangements. Likewise, NHA is not responsible for procuring commodities. It can and should, however, consider how it can exert its influence on the market to improve quality and efficiency (this is not the same as driving prices right down[65] and with them driving suppliers out of the market and risking increasing the rates of substandard medications). NHA could, for example, incentivise, through preferred devices and medicines lists, better commodity prices and guaranteed quality for guaranteed minimum volumes/market size and with favourable payment arrangements for suppliers by empaneled providers. Such a move would require three things: (a) stringent quality controls, (b) enforcement of the preferred list over providers, and (c) ability to guarantee a minimum but sizeable market and favourable payment terms. It may also require that NHA is granted the legal powers to negotiate with suppliers.
Competitive bidding may be one way to achieve best prices (without the adverse effects of price capping) and guaranteed supplies. China’s recent experiment centralising procurement and running tightly regulated tenders across 11 cities (the 4+7 cities pilot) is a case in point.[66] Early reports suggest up to $850m in savings for the insurer and a boost for the bigger domestic suppliers. Tackling the medicines and devices market is no small feat but tackling OOP on drugs whilst ensuring minimum quality are critical to achieving the NHA vision. So, identifying the major commodity drivers of OOP spending (which accounts for over three-quarters of the total OOP) and including those in NHA-preferred lists with zero co-pay and at competitive prices for suppliers may be a win-win for NHA, Indian manufacturers, and, most importantly, beneficiaries.
What happens next? Some ideas for immediate and medium-term action
In the immediate future post-election, NHA and the Indian authorities ought to lay the foundations for a well-funded, dedicated mechanism set up to serve policy makers’ needs and to create an accountable mechanism for supporting evidence-informed decisions by NHA and SHAs.
NHA, in close coordination with state-level SHAs, can serve as an incubator for such an evidence-to-policy mechanism, building its own internal capacity to identify research, technical and data needs, commission, coordinate, quality assurance, present to decision makers and help act on the data research results, ideally drawing on the newly established HTAIn and its academic hubs across the country and tapping into networks of excellence including universities, ICMR centres, the NCG and others (e.g. CMC Vellore).
Other nations with successful UHC schemes have such dedicated capacity. Thailand’s UC has IHPP[67] and HITAP,[68] the latter informing listing decisions for services and technologies for the country’s universal coverage scheme. Mexico’s INSP is dedicated to capacity building in health and social policy and in multidisciplinary research for evidence informed social policies.[69] INSP evaluated Seguro Popular.[70] Brazil’s SUS has FioCruz[71] and the British NHS has a dedicated R&D institute, NIHR,[72] as well as NICE[73] to help it make (and defend) decisions about policies, technologies, and services.
Such a mechanism would have some immediate analytical tasks and also a remit to develop the methods and processes by which research and data will be sourced and applied to real policy decisions. Amongst the immediate tasks, one may wish to include a review of the current packages of services given the latter’s importance in driving quality and efficiency across the system. There is experience from other countries of such quick reviews, such as in the case of Vietnam, which refreshed its medicines list based mostly on criteria of clinical appropriateness.[74] France did a similar exercise in the early 2000s.[75]
It would also propose a blueprint to government as to how such analytical capacity ought to be organised; the relationship (including outsourcing vs. building internal capacity) with governmental, public, and private centres of research excellence across India and beyond; and lines of accountability and budgets.
After the first six months, a priority would be to launch a process for developing world-class methods and standard operating procedures to carry out a series of critical analytical tasks as discussed above, including:
-
Drive the review of the benefits packages and related tariff rates and increase defensibility of decisions whilst managing any backlash from interest groups. Develop a systematic, multi-stakeholder, transparent, and evidence-informed approach for developing more structured processes around costing (may build on the iDSI costing database), listing and delisting (e.g., add indications) and connection of HBP to provider payments and premiums/allocation formula;
-
Inform guidance on adjusting benefit capitations for medical inflation and population risk profiles;
-
Publish standard operating procedures for major activities including the adjustment of the benefits plan, its costing and rate setting;
-
Explore coordination with other existing schemes providing cover to the formal sector so as to reduce fragmentation.
The NHA analytical mechanism could eventually be spun off as an Indian “what works”[76] centre for insurance/assurance lab, with technical resource units at state level to support SHAs with implementation and in collaboration with major international and Indian universities to showcase impact of PM-JAY and course correct as needed and to produce global public goods for informing the global UHC movement. The functions of such a hub (NHA) and spoke (SHAs) structure could include:
-
Carrying out impact assessments, including on savings and health gains and rapid evaluations (and troubleshooting) for key cost-effective hospital-based care, like repair of congenital heart disease aimed at showing immediate but also longer-term impact on health and spending of the NHA offer.[77]
-
Performing data field assessment to prioritise those types of data needed for addressing policymakers’ questions
-
Informing continuous benefits package design and adjustment linked to costing at NHA and SHA level and to HTAIn/hubs
-
Establishing community of practice for sharing experiences and capacity building including with insurance-based countries such as Colombia, the Netherlands, and Indonesia and for exploring jointly with others regulatory frameworks for private payers (e.g. ANS in SUS/Brazil[78] and CMS in RSA[79]).
Concluding thoughts
India has kicked off a major tax-funded UHC reform with impressive early gains in covering the poor, providing hospital-based treatment, and generating efficiencies in claims processing that has enabled private participation in provision. Post-election, it will be vital to move quickly on a set of rules of the game and administrative adjustments that will assure that PM-JAY delivers on its promise to enhance access, reduce catastrophic out-of-pocket spend, and enhance value-for-money in its own expenditure, while serving as a force to leverage improved health with transparency and accountability. Linking of PM-JAY with primary healthcare through Health and Wellness Centres and other mechanisms will be critical to create a continuum-of-care approach.
[1] Narayanan, Nayantara, Nithya Subramanian, and Rohan Venkataramakrishnan. “The Election Fix: How will voters pick between Ayushman Bharat and a Right to Healthcare?” Scroll, March 2019. https://scroll.in/article/917623/the-election-fix-how-will-voters-pick-between-ayushman-bharat-and-a-right-to-healthcare
[2] “How India Eradicated Polio.” WHO Global Polio Eradication Initiative, November 2018. http://polioeradication.org/news-post/how-india-eradicated-polio-challenges-and-lessons-learned/
[3] WHO Global Health Expenditure database. http://apps.who.int/nha/database/ViewData/Indicators/en
[4] In addition to the RSBY, Karnataka—one of the best performing states in health—ran the Suvarna Arogya Suraksha Trust (SAST) as a third-party administrator to implement the Vajpayee Arogyashri Health Assurance Scheme (VAS) for BPL families. Besides the VAS, several other schemes operate: the Rajiv Arogya Bhagya scheme, the RBSK scheme, the Cochlear Implant scheme, the Jyothi Sanjeevani scheme, Indira Suraksha Yogana scheme, and the Mukhyamantri Santwana Harish scheme.
[5] Rao, Nivedita. “Who is paying for India’s healthcare?” The Wire, April 2019. https://thewire.in/health/who-is-paying-for-indias-healthcare
[6] LaForgia and Nagpal (2012) examined the features of three central-level schemes and six state schemes between 2007 and 2012, finding that about 20 percent of the population benefitted from GSHIS, accounting for about 6 percent of total public spending on health in 2009-10. The authors also found wide variations in benefits coverage; all currently exclude preventive and primary care services, and most focus on higher-end tertiary inpatient care, particularly surgical procedures. RSBY, the largest government-sponsored health insurance program, covers frequent secondary-level inpatient procedures, such as hysterectomy, gall bladder removal and cataract surgery, per claims data (Morton et al 2016). In terms of immediate outcomes, a recent systematic review of 14 evaluations of GSHIS (Prinja et al 2017) found that most schemes increased healthcare utilization but did not necessarily reduce out-of-pocket spending on health, while only one scheme in Karnataka state (VAS, see below) was found to have caused relatively lower levels of mortality from conditions covered by the scheme (Sood et al 2014).
[7] Bhatt, Pallav and Digvijay Singh Sandhu. “Effect of the National Rural Health Mission on institutional deliveries and related out-of-pocket spending by the poor.” BMJ Global Health, July 2016. https://gh.bmj.com/content/1/Suppl_1/A5
[8] Gupt, Anadi, P. Kamraj, Prabhdeep Kaur, and B. N. Murthy. “Out of pocket expenditure for hospitalization among below poverty line households in District Solan, Himachal Pradesh, India, 2013.” PLoS ONE, February 2016. https://doi.org/10.1371/journal.pone.0149824 ; Sood, Neeraj and Zachary Wagner. “Social health insurance for the poor: Lessons from a health insurance programme in Karnataka, India.” BMJ Global Health, February 2018. http://dx.doi.org/10.1136/bmjgh-2017-000582
[9] Agrawal, Ritu, Salima Bhatia, and Amit Prasad. “The effect of the National Rural Health Mission on health services and outcomes for childbirth in India: A retrospective analysis of survey data.” The Lancet, volume 382, issue 11 (2013). https://doi.org/10.1016/S0140-6736(13)62172-8 ; Vellakkal, Sukumar, Ann Bowling, Pat Doyle, Shah Ebrahim, Adyya Gupta, Zaky Khan, Aaron Reeves, and David Stuckler. “Has India’s national rural health mission reduced inequities in maternal health services? A pre-post repeated cross-sectional study.” Health Policy and Planning, volume 32, issue 1 (2017): 79-90. https://doi.org/10.1093/heapol/czw100
[10] In addition to substantial investment through NHM in strengthening public facilities, health insurance schemes have also played an important part where a large part of the claims was paid to public facilities.
[11] Indian Council of Medical Research, Public Health Foundation of India, and Institute for Health Metrics and Evaluation. “India: Health of the Nation's States”. IHME, November 2017. http://www.healthdata.org/policy-report/india-health-nation’s-states
[12] Gupta, Shuchita, Shyama Nagarajan, Vinod K. Paul, and Namrata Yadav. “The National Rural Health Mission in India: Its impact on maternal, neonatal, and infant mortality.” Seminars in Fetal and Neonatal Medicine, volume 20, issue 5 (2015): 315-320. https://doi.org/10.1016/j.siny.2015.06.003
[13] Angell, Blake J, Anadi Gupt, Stephen Jan, Vivekanand Jha, and Shankar Prinja. “The Ayushman Bharat Pradhan Mantri Jan Arogya Yojana and the path to universal health coverage in India: Overcoming the challenges of stewardship and governance.” PLoS Medicine, volume 16, issue 3 (2019). https://doi.org/10.1371/journal.pmed.1002759
[14] For rural areas, six deprivation criteria out of seven total criteria (D1 to D5 and D7) were used. For urban areas, thirteen occupational categories were used for identifying beneficiaries under PM-JAY.
[15] Keane, Michael and Ramna Thakur. “Health care spending and hidden poverty in India.” Research in Economics, volume 72, issue 4 (2018): 435-451. https://doi.org/10.1016/j.rie.2018.08.002
[20] See: www.worldbank.org/en/news/opinion/2013/12/20/brazil-sus-unified-public-healthcare-system-new-study
[21] See: http://www.worldbank.org/en/results/2015/02/26/health-coverage-for-all-in-mexico ; The new president of Mexico recently announced the cancellation of the scheme due to concerns, amongst others, over sourcing medicines. (“Se cancelara el Seguro Popular; se gastaban 90 mil mdp en medicinas: AMLO.” El Sol de Mexico, April 2019. https://www.elsoldemexico.com.mx/mexico/sociedad/se-cancelara-el-seguro-popular-se-gastaban-90-mil-mdp-en-medicinas-amlo-3285510.html)
[23] World Bank Universal Health Coverage Study Series. http://www.worldbank.org/en/topic/health/publication/universal-health-coverage-study-series
[24] Intergovernmental Fiscal Transfers for Health Working Group. “Power to the States: Making fiscal transfers work for better health”. Center for Global Development, December 2015. /publication/power-states-making-fiscal-transfers-work-better-health
[25] “OECD Reviews of Health Systems: Colombia 2016.” OECD, December 2015. https://www.oecd.org/health/oecd-reviews-of-health-systems-colombia-2015-9789264248908-en.htm
[26] Escobar, Maria-Luisa, Ursula Giedion, Antonio Giuffrida, and Amanda Glassman. “From Few to Many: Ten Years of Health Insurance Expansion in Colombia.” Brookings, January 2010. https://www.brookings.edu/book/from-few-to-many/
[27] Goddard, Maria and Rowena Jacobs. “Social health insurance systems in European countries: The role of the insurer in the health care system: A comparative study of four European countries.” University of York, June 2000. https://www.york.ac.uk/che/pdf/op39.pdf
[28] Sharma, Neetu Chandra. “Centre seeks to boost public health spending to 2.5% of GDP by 2025.” Live Mint, December 2018. https://www.livemint.com/Politics/I7KXpCYJ5D7LQhEaQku9EL/Centre-seeks-to-boost-public-health-spending-to-25-of-GDP.html
[29] Narayanan et al.
[30] Clarke, Lynda, Lalit Dandona, Anamika Pandey, and George B Ploubidis. “Trends in catastrophic health expenditure in India: 199 to 2014.” WHO Bulletin, volume 96, issue 1 (2018): 18-28. http://dx.doi.org/10.2471/BLT.17.191759
[31] Angell et al.
[32] See a recent analysis on insurance, OOP and financial risk protection here: https://doi.org/10.1371/journa l.pone.0211793
[33] Sahu, Prasanta. “Daily hospitalization under PMJAY may double by January.” Financial Express, November 2018. https://www.financialexpress.com/money/insurance/daily-hospitalisation-under-pmjay-may-double-by-january/1398744/
[34] Bhuyan, Anoo. “Government 'freezes' health insurance rates, ignores private hospitals' protests.” The Wire, June 2018. https://thewire.in/health/government-freezes-health-insurance-rates-ignores-private-hospitals-protests
[35] “Modi’s Ayushman Bharat pushing hard to get private hospitals on board; NHA sends invites.” Financial Express, November 2018. https://www.financialexpress.com/economy/modis-ayushman-bharat-pushing-hard-to-get-private-hospitals-on-board-nha-sends-invites/1393828/
[36] Raghavan, Prabha and Aman Sharma. “Govt seeks help from IT biggies to make Ayushman insurance schemes fraud free.” Economic Times, September 2018. https://economictimes.indiatimes.com/tech/ites/govt-seeks-help-from-it-biggies-to-make-ayushman-insurance-scheme-fraud-free/articleshow/65801415.cms?from=mdr
[37] Ahuja, Rajeev. “PM-JAY: Can it rise to the challenge?” Financial Express, December 2018. https://www.financialexpress.com/opinion/pm-jay-can-it-rise-to-the-challenge/1429238/
[38] Rana, Kumar. “Ayushman Bharat's declared measures seem neither adequate nor practical.” The Wire, October 2018. https://thewire.in/health/ayushman-bharats-declared-measures-seem-neither-adequate-nor-practical
[39] Gupta, Prachi. “How to bring private hospitals on-board Modi’s Ayushman Bharat: FICCI has this suggestion.” Financial Express, January 2019. https://www.financialexpress.com/industry/how-to-bring-private-hospitals-on-board-modis-ayushman-bharat-ficci-has-this-suggestion/1443523/
[40] iDSI Reference Case. https://www.idsihealth.org/resource-items/idsi-reference-case-for-economic-evaluation/
[41] Bauhoff, Sebastian, Matthew Morton, Somil Nagpal, and Rajeev Sadanandan. “India’s largest hospital insurance program faces challenges in using claims data to measure quality.” Health Affairs, volume 35, issue 10 (2016): 1792-1799. https://doi.org/10.1377/hlthaff.2016.0588
[43] See: https://icmr.nic.in/sites/default/files/reports/Report%20of%20Health%20Technology%20Assessment%20(HTA)-%20Stakeholders%27%20Consultative%20Workshop.pdf ; https://gh.bmj.com/content/2/2/e000259
[44] “Outcome Report on ‘Health Technology Assessment of intraocular lenses for treatment of age-related cataracts in India.’” HTAIn Secretariat, July 2018. https://dhr.gov.in/sites/default/files/htaincataract_0.pdf
[47] Chalkidou, Kalipso, Francoise Cluzeau, Saudamini Dabak, Laura Downey, Alia Cynthia Gonzales Luz, Abha Mehndiratta, Songyot Pilasant, Yot Teerawattananon, and Sitaporn Youngkong. “Budgeting for a billion: applying health technology assessment (HTA) for universal health coverage in India.” Health Research Policy and Systems, volume 16, issue 115 (2018). https://doi.org/10.1186/s12961-018-0378-x
[48] See: https://www.gob.cl/en/news/10-years-of-auge-achievements-guarantees-and-how-the-health-plan-works/
[49] “Amartya Sen: Ayushman Bharat neglects primary healthcare, sector needs radical change.” Indian Express, February 2019. https://indianexpress.com/article/business/amartya-sen-ayushman-bharat-neglects-primary-healthcare-sector-needs-radical-change-5603964/
[50] Rao, K. Sujatha. “Healthcare system hanging on hospital insurance without foundation of primary care is unsustainable.” Indian Express, April 2019. https://indianexpress.com/article/opinion/columns/india-healthcare-medical-insurance-bjp-5665733/ ; Singh, Rajesh. “Ayushman Bharat a game-changer, but concerns have to be addressed.” Vivekananda International Foundation, October 2018. https://www.vifindia.org/article/2018/october/05/ayushman-bharat-a-game-changer ; Raman, Sumanth. “Why Ayushman Bharat will not work.” New Indian Express, October 2018. http://www.newindianexpress.com/opinions/2018/oct/06/why-ayushman-bharat-will-not-work-1881816.html
[51] “Amartya Sen: Ayushman Bharat neglects primary healthcare, sector needs radical change.”
[52] Bhushan, Indu. “In Ayushman Bharat, primary and secondary healthcare complement each other.” Indian Express, March 2019. https://indianexpress.com/article/opinion/columns/ayushman-bharat-scheme-amartya-sen-healthcare-sector-5636552/
[53] Forman, Rebecca and Amanda Glassman. “Setting Universal Health Coverage priorities: India and dialysis.” Center for Global Development, July 2016. /blog/setting-universal-health-coverage-priorities-india-and-dialysis
[54] See the advice by the Elders here: https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(18)32387-0/fulltext
[55] “A tiered health-care delivery system for China.” The Lancet, volume 393, issue 10177 (2019). https://doi.org/10.1016/S0140-6736(19)30730-5
[57] Pramesh C. S. et al. “Choosing Wisely India: Ten low-value or harmful practices that should be avoided in cancer care.” The Lancet Oncology, volume 20, issue 4 (2019). https://doi.org/10.1016/S1470-2045(19)30092-0
[58] “Outcome Report on ‘Health Technology Assessment of intraocular lenses for treatment of age-related cataracts in India.’”
[59] See an ex ante HTA proposal for pulling a TB treatment regimen into the global market based on the value of it to emerging economies with a TB burden, such as India, here: /sites/default/files/MVAC-Blueprint-for-Consultation-2019-02-28.pdf
[60] Chalkidou, Kalipso and Janeen Madan Keller. “Healthcare systems as intelligent payers: What can the global health community learn from the English National Health Service?” Center for Global Development, February 2018. /publication/healthcare-systems-intelligent-payers-what-can-global-health-community-learn-nhs
[61] OECD Health Care Quality Indicators. https://stats.oecd.org/Index.aspx?DataSetCode=HEALTH_HCQI
[62] Appleby, John and Nancy Devlin. “Getting the most out of PROMs: Putting health outcomes at the heart of NHS decision-making.” The King’s Fund, 2010. https://www.kingsfund.org.uk/sites/default/files/Getting-the-most-out-of-PROMs-Nancy-Devlin-John-Appleby-Kings-Fund-March-2010.pdf
[63] “China policies to promote local production of pharmaceutical products and protect public health.” WHO, 2017. https://www.who.int/phi/publications/2081China020517.pdf
[64] “Brazilian industrial and innovation complex in health: Productive Development Partnerships (PDP) to guarantee access to health technologies in Brazil.” WHO, n.d. https://www.who.int/medical_devices/global_forum/J01.pdf
[65] Dean, Emma C. B. “Impacts of pharmaceutical price controls on pricing, sales, and market-level quality: Evidence from India.” University of Pennsylvania, 2018. https://repository.upenn.edu/dissertations/AAI10793313
[66] Johnson, Jim, Xin Tao, and Lu Zhou. “China takes significant steps to consolidate generic drug industry and lower prices.” Hogan Lovells, December 2018. https://www.hlregulation.com/2018/12/10/china-takes-significant-steps-consolidate-generic-drug-industry-lower-prices/
[74] “Reaching the low-hanging fruits of Vietnam’s Health Benefit Package reform.” HITAP, March 2017. http://www.hitap.net/wp-content/uploads/2017/02/PB_HiU_vietnam_final_forweb_22_feb_2017.pdf
[75] Pichetti, Sylvain and Catherine Sermet. “Analysis of the impact of drug delisting in France between 2002 and 2011.” IRDES, August 2011. https://www.irdes.fr/EspaceAnglais/Publications/IrdesPublications/QES167.pdf
[76] See the UK “What Works Network” here: https://www.gov.uk/guidance/what-works-network
[77] See an evaluation of the Chilean AUGE scheme here: https://www.healthaffairs.org/doi/full/10.1377/hlthaff.2010.0972
Rights & Permissions
You may use and disseminate CGD’s publications under these conditions.