In June 2021 at the G7 summit, Dr. Tedros Ghebreyesus, director-general of the World Health Organization (WHO), offered a challenge to the world: “To truly end the pandemic, our goal must be to vaccinate at least 70 percent of the world’s population by the time you meet again in Germany next year.” This target became WHO strategy and then rapidly incorporated into national targets around the world. The target is also used by advocates to track progress and raise monies.
At the time, the 70 percent coverage goal made sense. Many countries were reeling from their second major COVID wave, and the vaccines were highly efficacious at preventing hospitalization and death from the circulating Delta variant. Further, the evident inequity in vaccination coverage was a moral and political embarrassment—while 43 percent of people in high-income countries had received at least one vaccine dose by mid-2021, less than 1 percent of people had in low-income countries. The 70 percent goal provided clarity, equality, and ambition, and likely catalysed global leaders to increase financing support to Covax to meet its goal of providing sufficient supply for 40 percent coverage in its partner countries by the end of 2021.
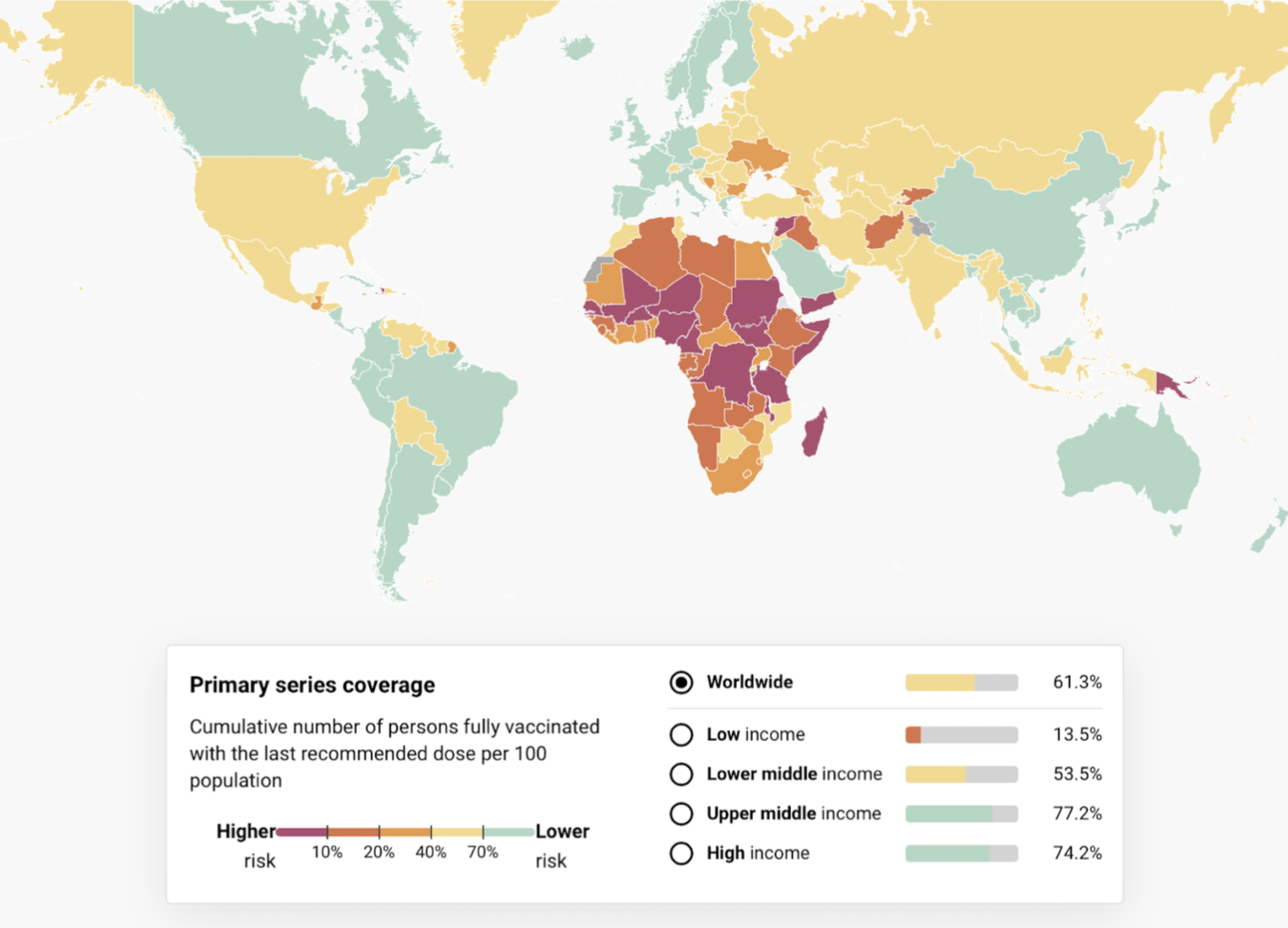
However, as we approach this year’s G7 summit on June 26-28, the 70 percent target has been missed in most countries and almost all African countries (see Fig 1). Still 16 percent of people in low-income countries have received one dose and 14 African countries have vaccinated less than 10 percent of their population. While slow roll-out was initially caused by vaccine supply shortages, the slow rhythm of expansion in these countries now relates more to the priority given by governments to the activity, vaccine hesitancy as well as a lack of financing and other capacity for delivery.
Figure 1. Country progress to achieve 70% vaccination coverage by mid-2022
Source: covid19globaltracker.org
Against this backdrop, the crucial question is whether, at the G7 summit and beyond, global leaders should recommit to the 70 percent coverage goal. Our answer is a resounding “no.” We believe the 70 percent target is no longer fit for purpose. Instead, a more targeted approach is needed to protect those at greatest risk. Three reasons justify our call for a serious re-think:
1. The virus has changed
Omicron and its subvariants, first detected in South Africa and Botswana in early November 2021, are now the predominant strains of the virus globally. These variants are more contagious but have resulted in less morbidity and mortality than earlier strains, and existing vaccines are less effective at preventing transmission. The protection that is afforded by vaccines also seems to wane relatively quickly. These developments imply that achieving herd immunity through vaccination is unlikely. In addition, seroprevalence of SARS-nCoV-2 is much higher than reported cases suggest and thus many people have some degree of immunity through exposure to the virus. The dynamics between rising immunity due to exposure or vaccination, the timing of the waning of that immunity, and the evolution of the virus means the situation will continue to change over time. Future scenarios could include the emergence of a dangerous variant, against which currently available vaccines may or may not be effective. If effective, rapid redeployment of existing vaccines might be an option for the future while new vaccines designed specifically to combat the new threat are developed and made available. But a simple population-wide target of 70 percent in the Omicron era has lost its epidemiological purpose to limit ongoing transmission, so the aim of vaccination is no longer herd immunity but reduction in serious illness and death in the near term.
2. Countries should maximize value for money in reduction of illness and death
The drive toward achieving large-scale population coverage regardless of age or health status may be undermining efforts to prioritise those who should be vaccinated first: health workers and those at higher risk of severe outcomes. Moreover, resources used in vaccinating people against COVID have an opportunity cost. Whether “fresh” money or existing health system capabilities, resources used for COVID vaccination are therefore not used to deliver some alternative health services or other government efforts. Using this standard, research led by the International Decision Support Initiative (iDSI) and partners confirms the diminishing value of higher levels of coverage of COVID-19 vaccination in African countries, compared to alternative uses of health spending, suggesting that for low income countries, only early vaccination with low-cost vaccines would have been cost-effective from a national perspective. In this analysis, vaccination at large scale was only cost-effective for one in three low-income African countries by the end of 2021, and declining—in this case likely due to the rise in exposure-driven immunity over time, though waning immunity was not modelled. Additional analysis in Kenya that did include waning immunity finds that “With prior exposure partially protecting much of the Kenyan population, vaccination of young adults may no longer be cost-effective.” Drawing on the above studies, Africa CDC argues that "timing and targeting will be critical considerations for many African countries’ vaccine programmes. Data from country case studies showed that a very fast rollout to the most vulnerable, even if it only covers between 25-40% of the population, has a massive effect on reducing deaths and containing costs.”
3. Donors' contributions have been too little, too late
The supply of COVID-19 vaccines to low-income countries did not come early enough, as high-income countries sought to secure (more than) enough for their own populations and timely financing for lower-income countries was not secured. Achieving 70 percent COVID vaccine coverage using only domestic finances was never a likely option for many low-income countries and as expected, much of the supply of COVID-19 vaccines to African countries has come through Covax, AVATT, or bilateral donations.
Donations aiming to support national priorities also have an opportunity cost and since vaccinations are counted as official development assistance (ODA), countries are effectively foregoing other aid investments. Therefore, the above arguments about value for money also broadly apply to donations or subsidies for vaccines. The remaining financing gap to achieve sufficient vaccine for 70 percent coverage in Covax-eligible countries was recently estimated to be $3.7 billion. While some COVID-19 vaccine financing will remain important to protect priority groups, some of this would be better spent on other essential health services.
Beyond direct protection of local populations, global institutions and donors are concerned with global health security and the potential threat of continued circulation of virus leading to a new virulent pandemic strain. In economists’ terms, there are externalities to population vaccination in low- and middle-income countries that potentially include systemic threats to societies and economies around the world.
To date, the economic cost of the COVID pandemic is estimated to exceed $12.5 trillion. While achieving 70 percent vaccine coverage is no longer the right strategy to prevent transmission of existing variants, pandemic preparedness is clearly important. Future dangerous variants are entirely possible, and the risks posed by other emergent pathogens are equally real. Recommendations for what form pandemic preparedness should take are available elsewhere, but it should be clear that moving away from the goal of 70 percent vaccine coverage should not mean relaxing into insouciance.
The way forward
National leaders will want to get the best bang for the buck for their populations. While what the future holds for COVID remains uncertain, for many countries this now means targeted vaccination including boosters, and potentially omicron-specific boosters, not 70 percent scale to the entire population. Moving forward:
- Countries must be supported to set their own targets, focus vaccines on priority groups first, and to prepare for the next variant.
- If a global target is desired to continue to galvanise actions, a goal of vaccinating all health workers and vulnerable groups in all countries would be more effective than a fixed percentage.
- Specifically, ACT-A agencies should reconsider whether the identified $3.7 billion funding gap for vaccine supply is best allocated to existing vaccine procurement or whether it could be more effective allocated across other ACT-A priorities.
Leaders should not lose sight of pandemic preparedness. While vaccination at scale may not be a priority with the current epidemiology, we must be better prepared to act quickly and equitably in response to the next dangerous variant or a new pandemic threat.
Disclaimer
CGD blog posts reflect the views of the authors, drawing on prior research and experience in their areas of expertise. CGD is a nonpartisan, independent organization and does not take institutional positions.