The global commitment to universal health coverage—target 3.8 of the Global Goals for Sustainable Development—is as ambitious as it is energizing. Ensuring everyone, everywhere around the world has access to quality health care without being forced into poverty will require stronger health systems that generate better patient services and improve people’s health. And, to that end, investments in hospitals and their performance will be key.
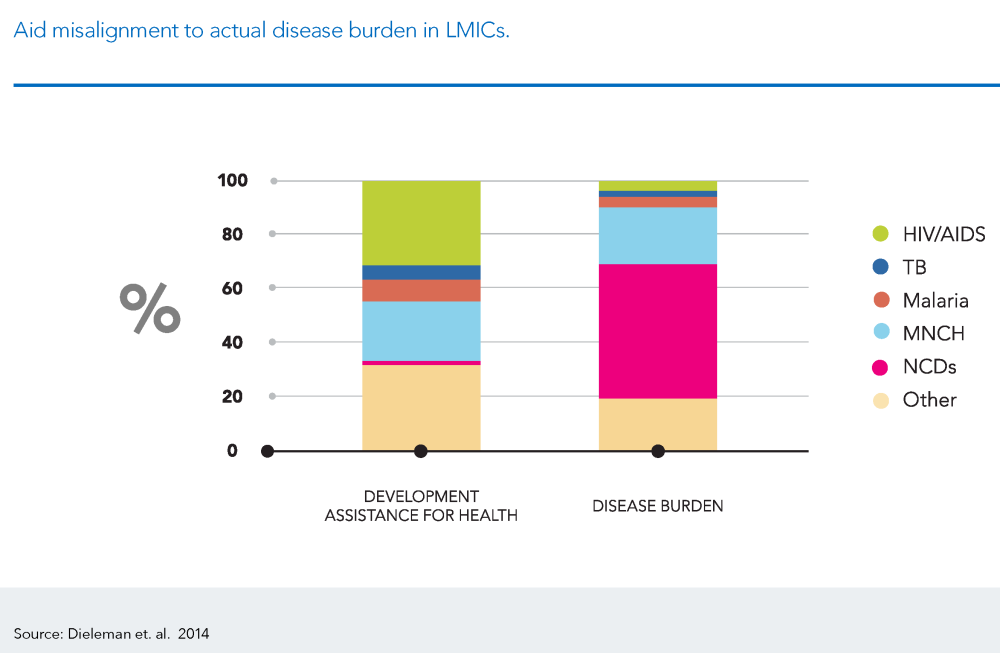
UHC is about timely, appropriate and high quality services at an affordable price, yet hospitals are often overlooked by country governments and donors alike. This needs to change given the shift in disease burden—whereby cardiovascular disease, cancer and trauma, rather than infectious diseases, now dominate the burden of disease even in the poorest countries. Cancer and cardiovascular disease each claim more lives in Sub-Saharan Africa than AIDS, tuberculosis and malaria combined—although the latter remain the focus of funders. Health investment priorities must shift to meet the changing disease profile.
If we continue to give little attention to upgrading and integration of hospitals and their services, low- and middle-income countries will remain ill-equipped to meet their commitment to UHC. Sticking with the status quo leaves modernization and expansion of hospitals to the private sector, which typically skews investments to the upper and middle classes and often increases inequalities within and across countries. For example, the boom in private hospital construction in many middle income countries in East Asia compensates for the lack of public investment in hospital services. But these private hospitals are used by the wealthy who can afford their services, while the poor are relegated to seek care at public hospitals. The poorest citizens in low- and middle-income countries ultimately suffer the most.
Although bilateral and multilateral donors focus almost exclusively on primary health care to meet UHC goals, and philanthropic institutions like the Bill & Melinda Gates Foundation have followed suit, this strategy falls short of the needs and preferences of country governments and their citizens. And it undermines the quality of the evolving health care system.
First, countries are clearly concerned about the lack of hospital investments. This is most evident through the fact that countries are increasingly seeking support from the multilateral development banks and their private sector arms, such as the International Finance Corporation, to make new investments.
Middle income countries moving towards UHC, such as China, Brazil and Nigeria, already spend 70 percent of their health budgets on hospital care. Improving hospitals’ efficiency and quality, as well as integration with primary care, is critical to raising performance. It would also be cost effective to do so. Without hospitals, primary health care services, and investments made in hiring staff or new equipment, lack a point of reference and an effective referral network. If hospitals are dysfunctional, services at all levels suffer.
Second, the specialized expertise and support of hospital care remains central to the treatment of trauma, cancer, and other chronic diseases—which require new and more costly health care strategies. Although primary health care remains important, building integrated care networks that link hospitals to outpatient services can offer cost effective and critical services to people increasingly dependent on them.
As countries and donors seek to manage the rise of non-communicable and chronic diseases, prioritizing the building-up of health system capacity and improving health system performance can bring healthy returns. As I’ve written about before, this means renewing their efforts to upgrade health care systems, investing in secondary and tertiary facilities, and integrating care across inpatient and outpatient services. Furthermore, investments should be made to improve hospital leadership—an indispensable tenet of quality hospitals, management, and health care.
Without putting efforts towards hospitals, UHC goals risk becoming hollow exhortation rather than empowering targets. That’s why I’m helping host an event at CGD on December 7 to launch a new report, Better Hospitals, Better Health Systems, Better Health. I hope you’ll join us for a discussion on the critical issues around and importance of improving and reforming health systems and hospitals in low- and middle-income countries, where it’s needed most. (Register here)
CGD blog posts reflect the views of the authors, drawing on prior research and experience in their areas of expertise.
CGD is a nonpartisan, independent organization and does not take institutional positions.