As more and more low-income countries report COVID-19 infections, there are urgent concerns of whether health systems will be able to cope. One particular worry is whether health workers will be protected at the frontlines of diagnosing and treating infected patients. Across the world, doctors, nurses, community health workers, and others are at elevated risk of infection and mortality. They are also a crucial asset to battling the pandemic. In Europe, infections among medical staff have already generated worker shortages. In low-income countries, health workers are scarce even in good times: the average low-income country has 0.2 physicians and 1 nurse per 1,000 people, compared to 3 and 8.8 in high-income countries. And while shortages of protective equipment and materials have become a major issue in high-income countries, the picture is bleaker in low-income countries
The Ebola crisis demonstrated both the importance of protecting health workers and the struggle health systems of low-income countries face in providing adequate protective equipment and infection prevention to protect their health workforces. Health workers are disproportionally at risk of infection and death, and, without adequate protective equipment, Ebola killed 8 percent of health workers in Liberia and about 7 percent in Sierra Leone. In addition to causing substantial loss of life, that deprived these health systems of a crucial asset to fight the current pandemic (and future ones).
Many health systems lack basic infection prevention and personal protective equipment
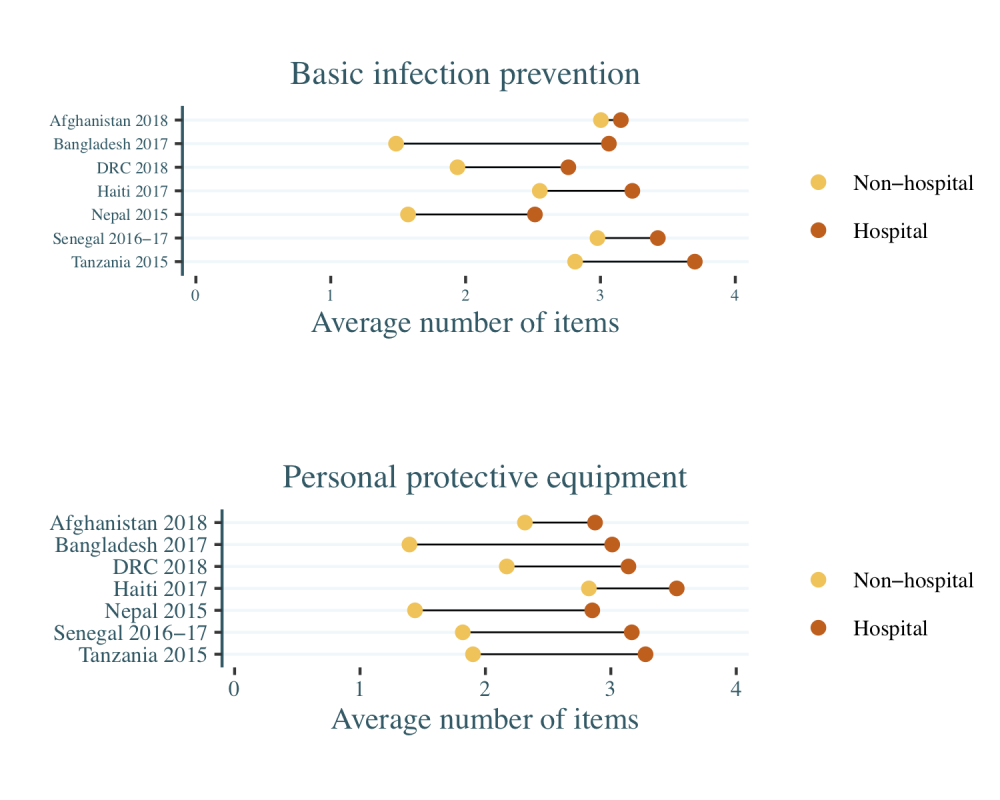
Using data from recent facility surveys (Service Provision Assessments), we examined the availability of basic infection prevention (BIP) materials and personal protective equipment (PPE) in health facilities in seven low- and low-middle income countries.
We use a shortened list of BIP consisting of four items: guidelines for infection prevention, pourable water and soap or hand disinfectant, surface disinfectant, and a waste bin. Per World Health Organization (WHO) guidance, PPE also consists of four items for those in direct contact with patients: gloves, face masks, gowns or aprons, and eye protection. These survey measures capture general availability but not whether supplies are adequate in quantity or quality, so they give an overly optimistic picture of facilities’ preparedness.
The prospects for protecting health workers are grim, especially for lower-level facilities such as clinics and health centers that often serve as the first point of contact with the health system (Figure 1). Across the seven countries, hospitals have an average of 3.1 out of the 4 items that make up each of BIP and PPE, whereas lower-level facilities average just 2.3 BIP items and 2 PPE items. Tanzanian and Haitian hospitals are the best equipped with BIP and PPE items respectively, while Nepalese hospitals are the least well-equipped in both items of the seven countries.
Figure 1. Availability of basic infection prevention materials and personal protective equipment in seven countries
The data for Bangladesh, DRC, Haiti, Nepal, Senegal, and Tanzania are nationally representative, whereas the Afghanistan sample covers seven urban areas; all estimates use facility sampling weights
Availability of specific items is highly variable (see tabulations for each item here). Among the BIP items, handwashing items and surface disinfectants were available in almost all hospitals but only in about 80 percent of lower-level facilities, while guidelines for infection prevention were frequently missing. Of the PPE items, gloves were available in almost all hospitals and in 9 out of 10 lower-level facilities. Face masks were generally available in hospitals but not non-hospitals: less than a third of clinics and health centers in Bangladesh, the Democratic Republic of Congo (DRC), Nepal, and Tanzania had any face masks. Eye protection was the least available item, present in an average of 37 percent of hospitals and 9 percent of clinics and health centers across the seven countries.
Plans to protect the health workforce are deficient or absent in many low-income countries
Even where inventory of key protective gear and infection prevention is available, it is unclear how health systems will be able to cope with increased demand for these items once infections rise. Most of the countries we reviewed score low on preparedness dimensions that are relevant to the health workforce, according to external evaluations on International Health Regulations (IHR), a set of international rules to prevent the spread of diseases (see Table 1). Most countries have an applied epidemiology training program in place and some human resources available to implement the IHR core capacity, but are lacking on other measures. Despite the DRC’s experience with the Ebola outbreak, the country still scored low on the most dimensions of preparedness, including medical countermeasures and personal deployment and risk communication plans.
Table 1. Selected capabilities to implement International Health Regulations (IHR) with regards to protecting the health workforce (range from 1 = “no capacity” to 5 = “sustainable capacity”)
| Category | Item | Afghanistan | Bangladesh | DRC | Senegal | Tanzania |
|---|---|---|---|---|---|---|
| Workforce development | Human resources available to implement IHR core capacity requirements | 1 | 3 | 2 | 3 | 3 |
| Applied epidemiology training program is in place | 2 | 4 | 4 | 4 | 4/2. | |
| Workforce strategy | 2 | 3 | 3 | 2 | 2/3. | |
| Preparedness | A multi-hazard national public health emergency preparedness and response plan is developed and implemented | 2 | 2 | 1 | 2 | 2 |
| Medical countermeasures and personnel deployment | A system is in place for sending and receiving medical countermeasures during a public health emergency | 2 | 1 | 1 | 2 | 2 |
| A system is in place for sending and receiving health personnel during a public health emergency | 2 | 1 | 1 | 2 | 2 | |
| Risk Communication | Risk communication plans | 2 | 2 | 1 | 1 | 2 |
| Internal and partner communication and coordination | 2 | 2 | 2 | 2 | 2 |
Source: WHO Joint External Evaluations. Haiti has completed a plan but it is not yet available online while Nepal has not created a plan.
Countries are struggling to improve infection control and provide workers with protective equipment
As high-income countries scramble to source crucial supplies like face masks—with calls to nationalize equipment producers or direct stimulus spending to invest this sector—low-income countries face even tougher choices. Their budgets are more limited, and they lack many local producers and have inefficient and insecure supply chains, with a substantial reliance on donors and multilaterals for procurement. Bangladesh’s large textile industry began production of nearly half a million pieces of PPE to be distributed to its health facilities last week, but this scale of production is not replicable in other low-income settings. The World Bank’s $12 billion support package might provide much-needed resources to purchase protective equipment and prop up basic infection control, though there are already concerns about price increases, hoarding, market manipulation, black markets and competition with high-income countries for these items.
Donors and multilaterals have not yet responded at sufficient scale
The global response to the looming health workforce crisis in low-income settings has been limited so far. WHO estimates that some 89 million masks and 76 million gloves may be needed in the coming months, and has called on manufacturers of PPE to boost production by 40 percent. Yet so far shipments of PPE to low-income countries are but a fraction of what’s needed: WHO has so far dispatched 0.5 million PPE sets; UNICEF has dispatched 4.3 million gloves, 100,000 N95 respirators and other PPE; philanthropist Jack Ma is donating 100,000 masks and 1,000 protective suits to each country in Africa, as well as 1.8 million masks to 10 Asian countries. It won’t be nearly enough.
These shortages in protective equipment and materials reflect the situation before the arrival of COVID-19 in any of these low-income countries. An inability to protect healthcare workers will not only lead to needless loss of lives, but also deplete already-stretched health systems. We can’t afford low-income countries to go through an experience like that of Liberia and Sierra Leone during the Ebola epidemic. To effectively fight COVID-19 in low-income countries—and hence globally—the international community needs to step up now to protect frontline health workers.
Disclaimer
CGD blog posts reflect the views of the authors, drawing on prior research and experience in their areas of expertise. CGD is a nonpartisan, independent organization and does not take institutional positions.
Image credit for social media/web: Photo by Martine Perret / UNMEER