Recently, my twitter feed contained a number of disappointing references to “Direct-To-Consumer Telehealth May Increase Access to Care But Does Not Decrease Spending.” People had hoped that this simple technology would save money. For my part, I was puzzled by the expressions of disappointment. I couldn’t fathom why anyone would have expected a different conclusion.
Health technologies can reduce healthcare spending. On average, they don’t. Prominent examples—like the way polio vaccines eliminated the need for iron lungs—seem to drive a common faith in healthcare technology as a tool to “cure” costly health systems. But it actually works the other way around—health systems (policies, institutions, and markets) and human responses to them determine whether these tools will (or won’t) increase spending.
The story of health technology, costs, and spending is not straightforward
The cost saving arguments for health technology look pretty compelling. Cost-effective prevention is an obvious candidate—measles vaccines improve health and eliminate demand for medical consultations. When lower cost health technologies (angioplasty) replace more expensive ones (coronary bypass surgery), you would think that spending should also decline.
But here’s the kicker…
Even when health technologies drive down costs, they might increase spending
Lowering the cost of prevention or treatment means that more people can afford it, that more plans cover it, and that more doctors prescribe it. Depending on how much the cost goes down and how much demand increases, overall spending could either fall … or rise. When lower costs lead to greater utilization and significant health gains, then the increased spending may be worth it. In other cases, increased utilization is of small (or even negative) benefit, and the increased spending is essentially wasted.
Whether technology raises or lowers overall spending is ultimately an empirical question. Studies find that technology generally leads to more spending (and better health). For example, when researchers looked at specific innovations like angioplasty, cataract surgery, and antidepressants, they found that treatment costs fell and utilization increased. What was the net effect? Higher spending and better health. Other studies using cross-country data have estimated that technological change accounts for as much as a quarter of all health spending growth. The size of the net effect is uncertain, but it is almost certainly positive.
What drives health technology?
The net effect of health technology on spending comes down to the way the health system—the interaction of markets, institutions, and public policy—encourages particular kinds of innovation. And here’s where healthcare is strange: the general rules and expectations regarding the power of markets to converge on efficient solutions is weak or even perverse when it comes to healthcare services.
In many markets, technologies converge on standards which increase efficiency. Consider how quickly the market for mobile phones has converged on two dominant operating systems (Android and Apple), how online sales converged on a few dominant e-commerce providers like Amazon and Ali Baba, or VCR standards beat out Betamax.
Healthcare markets don’t seem to work that way. For example, the US healthcare system has more market competition than any other, yet the US seriously lags other countries in the adoption of interoperable electronic health record platforms. In fact, as recently as 2007, less than one-fifth of US hospitals even had electronic data capture for inpatients, at a time when 12 other countries had a rate of over 90 percent. Other countries have moved toward more efficient use of healthcare technologies through a mix of public policies and private sector cooperation—not unlike efforts that went into agreeing on USB connectors or standards for docking with the international space station.
Markets also tend to drive technology toward the most profitable innovations, not necessarily the most cost-effective or the most useful ones. Hence the tendency to have more research and development on diseases of the rich rather than the poor and a greater willingness to pay for cures than prevention. Proprietary systems which gain rents from controlling information technology (and restrict the ability to scrutinize its effectiveness and safety) are also preferred by markets. By contrast, countries which use public health funding or rigorous private market regulation have a variety of additional tools for lowering drug prices and using cost-effectiveness criteria to influence which innovations are reimbursed by insurance systems or adopted by publicly-financed healthcare providers.
Technology isn’t the only source of innovation
The same issue of Health Affairs that included the study on telehealth, also evaluated several other healthcare delivery innovations. A major health insurance plan effort to improve quality and lower the costs of primary care failed to generate the expected savings. By contrast, a state-wide initiative in Oregon to move Medicaid enrollees into coordinated care programs lowered spending primarily by reducing inpatient utilization. The issue also pointed out where the US is heading, with a projected 20 percent of GDP going to healthcare by 2025 based on projections under current laws. Plans being floated under the new US administration put their faith in market forces to bend this curve—something we’ve never seen happen in healthcare anywhere in the world. By contrast, countries with high infant mortality could make large gains by adopting better technologies—if that is understood to mean more than new drugs or devices and encompass changes in management, organization and financing.
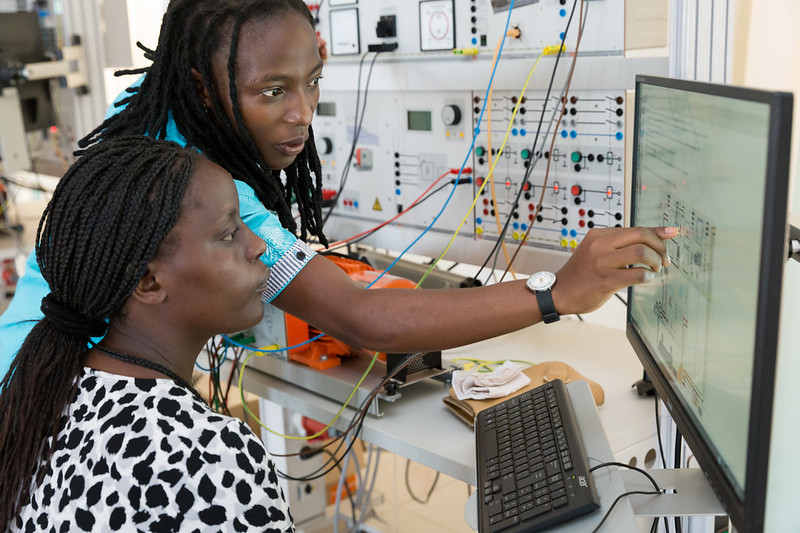
Telehealth is a great innovation for many countries, especially for those with dispersed rural populations. It is bound to be an important part of the health system toolkit for giving more people access to specialized diagnostics and improving patient screening in ways that reduce unnecessary service utilization. However, like all medical technologies, telehealth is just a tool. How this tool affects healthcare spending, health outcomes, and who gets care ultimately depends on the people (and the health system) that use it.
Thanks to Mike Brown and Janeen Madan for comments and feedback.
Disclaimer
CGD blog posts reflect the views of the authors, drawing on prior research and experience in their areas of expertise. CGD is a nonpartisan, independent organization and does not take institutional positions.