Recommended

Blog Post

CGD NOTES
Global health financing is due for a reckoning. Deteriorating macroeconomic conditions, alongside consequences of the war in Ukraine, and economic scars left by the COVID-19 pandemic have left many low- and middle-income countries (LMICs) with low or negative growth, increasing debt and highly uncertain incoming aid budgets. As a result, health spending is likely to drop or plateau, jeopardizing the path to post-COVID-19 recovery and universal health coverage (UHC). But there is an opportunity in every crisis and donors and LMIC governments should take advantage of this window to reimagine health financing. In this Policy Paper we propose an approach that meaningfully localizes decision-making, tackles the inherent challenges with aid, and increases value for money, helping to get us back on track to achieving UHC.
In this new compact for health financing, recipient countries and donors agree a model that allocates domestic finances ‘first’ to high priority, essential services, and aid is allocated to ‘top up’ additional services at the margin. This flips conventional aid logic on its head, to powerful effect. It means less fragmentation of recipient health systems, less volatility in funding of the highest priority services, less displacement of local resources, and more health for the money. It means a clearer, managed transition out of aid for flourishing health systems and, crucially, it means delivering on localization of global development with local decision makers back in the driving seat.
Figure 1. The marginal aid approach with health interventions ranked by cost-effectiveness

How the new compact could work in practice
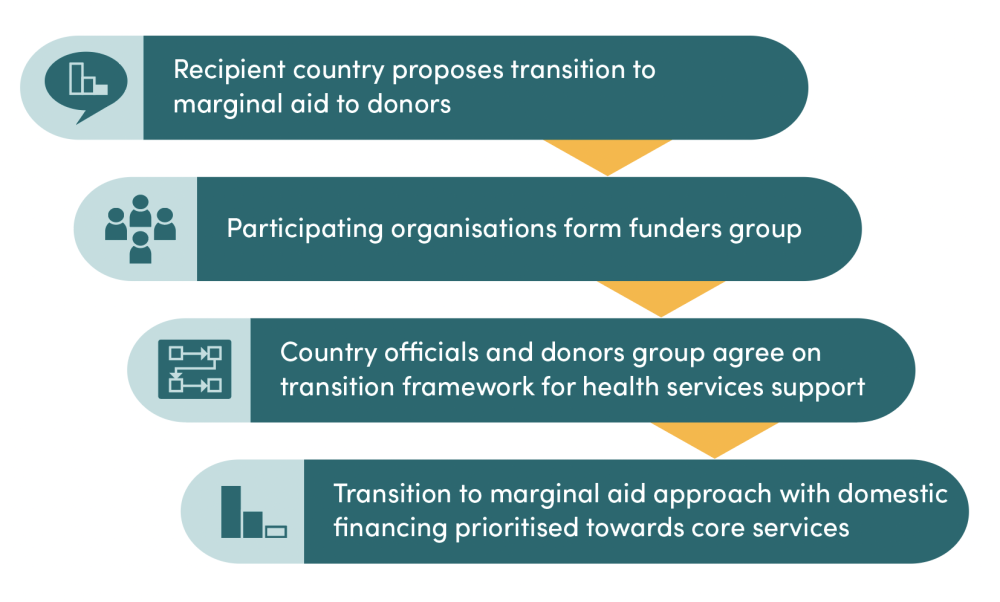
The new compact requires substantial trust and coordination between partners and government, as well as strengthened priority setting capabilities. Interested country governments and donors could build on existing health financing coordination structures including Sector-Wide Approaches. First, a country would state a policy intention to transition towards a marginal aid approach. Then, a country level health development partners group would be convened, and the country government and donors would agree a country-specific framework for a marginal aid financing. As part of this process, the interested country may request technical support to strengthen priority setting capabilities. At such a time that the country believes it has achieved a degree of success in priority setting and has effective systems to accurately differentiate higher and lower value services, it can propose to initiate the transition to a marginal approach (see Figure 2).
Figure 2. Steps towards marginal aid transition
Stakeholders are key to advancing the agenda
This is an ambitious vision for reform and all stakeholders in the financing of health services could play a part in advancing the agenda. For example:
Health Leaders in LMICs who believe a marginal aid approach would be helpful can call on donors to align and pilot a framework for financing health interventions at the margin.
Academics and researchers can help develop methods for a marginal financing approach. This will require developing frameworks for evidence-informed priority setting with multiple stakeholders and different payer perspectives. For example, today we have published a paper on how the marginal aid approach might work in terms of cost-effectiveness thresholds. Relatedly, technical assistance providers may be needed to support countries to make this transition, and to build their capacity for evidence-informed priority setting.
Global health donors, including multilateral funds, can be proactive in considering opportunities to shift their financial ways of working to a more constructive and sustainable marginal aid approach. They can avoid prioritising their own objectives, including claiming credit for the impact from the highest value services, and should be responsive to low- and middle-income countries requests to adopt a marginal aid approach.
Multilateral organisations with normative, governance and guidance roles, can work towards developing political or expert consensus on the importance of reforming global health financing and offer guidance on best practices. For example, in 2014 the World Health Assembly (WHA) agreed a statement in support of Health Technology Assessment and advocated for its role in achieving UHC. If methods for marginal aid gain traction the WHA could consider an analogous resolution. Regional organisations such as the African Union or African Centres for Disease Control could adopt similar guidance.
Change is inevitable. Will the global health community be able to seize the current moment to make a meaningful new compact on global health financing, and put aid in its rightful place?
Disclaimer
CGD blog posts reflect the views of the authors, drawing on prior research and experience in their areas of expertise. CGD is a nonpartisan, independent organization and does not take institutional positions.
Image credit for social media/web: Adobe Stock






