Global Burden of Disease (GBD) country rankings can strengthen the case of advocates at global and national levels for prioritising investment towards the major drivers of mortality and morbidity. But as discussed in our earlier blog post, when it comes to informing specific investment cases within these broader priorities, GBD data alone are not enough to allow consideration of trade-offs and of opportunity costs of alternative investment choices addressing the same problem. Further, the way the data are generated and presented makes it hard to get national researcher and policy maker buy-in (despite a broad engagement at country level and the introduction of “national GBDs”) as ownership remains with a Western centre of excellence (it is important to ensure coherence, standardisation and good quality, but not necessarily consistent with the whole idea of country ownership and local capacity strengthening).
The next step in using data to trigger action ought to be the generation, in conjunction with domestic stakeholders, of what we call below “super-local data.” For example, data that are granular enough to inform and defend usually very political local resource allocation decisions (and whose generation is in fact driven by those decision makers’ very political questions).
SDG data can make a strong case for addressing through reallocation and targeted interventions the geographical mismatch between need and resources (e.g. see here for an exposition of that mismatch when it comes to malaria in Nigeria) as long as the endogeneity between funding flows and outcomes over time can be controlled for.
However, for any analyses seeking to attribute causality between investment (quantity and quality) and achievement, as the GBD authors are promising, one may need much more granular “super-local” data, of the kind currently not included and hard to include in GBD, on things such as spending on interventions (which, by the way, can include population level public health programmes as well as individual pharmaceutical or diagnostic technologies) and their costs and benefits compared to the next best alternative for that specific setting. Further, only such “super-local” data could underpin a convincing case made to local payers and Treasuries for investment (or co-financing) using domestic resources, in effective interventions. And an accumulating body of such incremental decisions about, say, additions to the benefits’ package or to the medicines’ list, reimbursement rates and managed entry agreements, investing in primary care clinics for certain types of service provision or phased expansion of coverage to certain population groups, could then help tell a convincing story to domestic players about how GBD-informed targeting of investment can help drive better outcomes on the ground.
What’s included in super-local data
Super-local data include but are not limited to:
- local unit costs and resource use data: the Global Health Costing Consortium is a great start in terms of norm setting in methods and as a data repository, but it would need to go well beyond TB and HIV and include more granular resource-use data to be of use to national and subnational payers considering making listing, pricing and reimbursement decisions about technologies and services;
- an understanding of current practice, which, unlike the WHO CHOICE assumption, is rarely “the null”, i.e. a purely hypothetical and highly unrealistic situation where nothing is currently done in a country to address a certain problem (for a detailed critique see here);
- local patient and general population preferences for alternative health states, as opposed to extrapolating “value of life” estimates from the USA (see here for an attempt at setting priorities for spending for Bangladesh, somehow placing the value of life at exactly $8,503) or eliciting individuals’ values unrelated to national budgetary constraints (see here for one example of the latter, which places the value of an additional life year to over twice a developing country’s per capita GDP). Such approaches are frequently applied in global cost effectiveness and cost benefit evaluations. And by being completely disconnected from countries’ budgetary realities and hence highly hypothetical and unrealistic, they are perhaps less likely to convince national Treasuries to invest in health. In fact, were South Africa’s Treasury to adopt the value thresholds posited in the Global Health 2035 analysis, then scaling up four effective maternal, new-born and child interventions could absorb almost one quarter of the country’s public healthcare budget and still be deemed to be cost-effective;
- linked to the above, well calibrated decision rules, which are empirically rather than normatively based. Such granular data on inputs and outputs are currently hard to get at the country level in most LMICs (see here for such an attempt using country panel data and extrapolations);
- data on baseline distribution of attributes such as access to care, healthcare outcomes and spending coupled with an understanding of how new interventions may amend such distribution including on who the costs and benefits of introducing new interventions or scaling up existing ones, may fall. And, ideally, some societal (local) valuation of such changes. Extended CEA and distributional CEA are attempts at least at identifying the significant informational requirements of incorporating distributional concerns in coverage decisions, and have on occasions offered an exposition of trade-offs which could potentially inform actual policy decisions (e.g. neuropsychiatry and vaccines in Ethiopia or colorectal screening in the English NHS);
- context specific estimates of comparative clinical effectiveness of the interventions under consideration, ideally drawn from pragmatic trials carried out in the setting in which the adoption or scale up decision is about to be made, accepting that any progress towards the SDGs and UHC in particular that supports high-quality care “…will require that health systems are designed to integrate the delivery of health services with the generation of new knowledge about the effectiveness of these services.” (e.g. see here and here for a discussion of Learning Health Systems in LMICs)
- epidemiological evidence including incidence data for the major diseases and underlying risk factors that drive disease burden which must include NCDs and related risks such as high blood pressure. It could be that recent initiatives such as Resolve, could help fund research into filling this informational gap so that action to prevent NCDs can have an impact;
- evidence on likely mechanisms of successful adoption and scale up of cost effective interventions, of the kind provided by highly context sensitive realist evaluations, which seek to disentangle and interpret causal mechanisms interfacing with social and individual behaviour, in order to understand the mechanism of action of complex interventions. Though hardly applied in a systematic way to development interventions, this kind of realist evaluation is what Rob Baltussen and others describe when they talk about “evidence-informed deliberative processes” through which country allocation decisions are made en route to UHC.
A standardised Reference Case for economic analysis, widely used by high income countries’ payers when they make decisions on investing in services and technologies, includes most of the elements above and can serve as a useful reminder of methods and data gaps that must be filled if countries are to make their own informed decisions on spending for reaching UHC and meeting the SDGs.
The burden of collecting super-local data should not be placed squarely on the shoulders of the GBD team. As the researchers point out in their conclusion, “…GBD is not, and should not be, a replacement for investing in high-quality, routine health information systems that are crucial for measuring and evaluating SDG progress at national and subnational levels.” Other initiatives such as the recently launched Global Partnership for Sustainable Development Data or Paris21, may be better suited data collection and validation conduits. Perhaps a first step towards better quality relevant data would be committing some resources to implementing with select countries a Data Compact, a performance-based agreement between national and subnational governments, funders, technical agencies, private players and other stakeholders to reward country governments for progress made in producing and publishing better (more timely, more open, more accurate, more complete) data in one or two key areas. With better denominator data, and a stronger culture of good quality verifiable, openly available data, further progress towards sourcing and using more granular information such as costing data, could be achieved.
Such granular super-local data coupled with the technical and process support needed to bridge “the priorities ditch” for national authorities to apply them to difficult decisions locally, may change the nature of the discussion between Ministries of Health and National Health Insurance Funds on one hand, and National Treasuries, on the other. High profile calls to action and global cases of the billions of USD and millions of lives to be saved, made in prominent public health journals and conferences, may be less powerful unless there is evidence that national and subnational Ministries of Health:
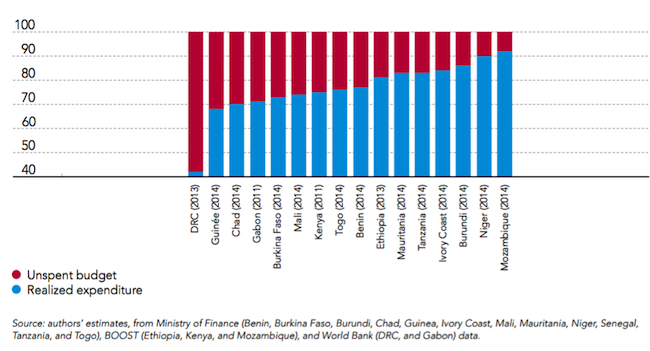
- can spend their already allocated budgets (health ministries in 16 SSA LICs have underspends ranging from 10 to 40 percent of their budgetary allocation—see the figure below);
Share of health budget spent and unspent, percent of total sector allocations
- do not commit publicly to major expansions in service and population coverage unless budgetary implications have been assessed and the fiscal space secured. In other words, unless they have demonstrable PFM competencies (e.g. over 20 Indian State governments have announced/are in the process of rolling out one or more of their own insurance schemes with variable “free healthcare” ceilings, limited/no coordination with the centrally managed RSBY, no analysis of current or forecast spending and a wide range of vague, rarely costed and often overlapping and all-encompassing benefits packages—see here for an analysis of the multitude of schemes across the country and here for the latest UHC announcement from State of Karnataka);
- are able to make convincing incremental, evidence-informed and locally relevant investment cases for individual technologies, services or programmatic reforms towards which growth monies ought to be channelled. Albeit not as impressive in terms of overall ROI and health impact, incremental analyses reflecting structured thinking as to how benefits packages ought to be expanded in terms of services and technologies and target subpopulations, at what price levels and to what cost to individuals, can boost confidence of Treasury officials in healthcare payer authorities making a case for more resources. Not unlike global investment cases and country rankings, cost effectiveness league tables of select technologies (see here for a recent example), devised outside the country with limited involvement and buy-in of local policy makers, do little to contribute to such confidence-boosting exercises between national Treasuries and national and subnational payer authorities.
In light of most countries transitioning away from aid dependence, monitoring progress towards the SDGs becomes all about holding the right people accountable and, at the same time, empowering the right people to act. The global perspective, whilst valuable, is perhaps no longer sufficient to trigger action at the local level.
Disclaimer
CGD blog posts reflect the views of the authors, drawing on prior research and experience in their areas of expertise. CGD is a nonpartisan, independent organization and does not take institutional positions.