Recommended
Global health is fundamentally undermined by power imbalances. Those who have the least access to health care, generally, have the least power to influence global health. This blog looks at one imbalance—the concentration of power in the hands of global health donors, in relation to governments and citizens of low- and middle-income countries (LMIC) that receive aid.
This a high-profile topic, partly driven by the inequities in the global COVID-19 response. For example, the Africa Centres for Disease Control and Prevention (Africa CDC) calls for African self-sufficiency in its new public health order, USAID continues to re-affirm commitment to its (struggling) localization strategy, and the UK Shadow Secretary for Foreign Affairs, David Lammy, has called for “modern equal relations of power, two-way partnerships based on respect and mutual trust.”
Four options for redistributing power
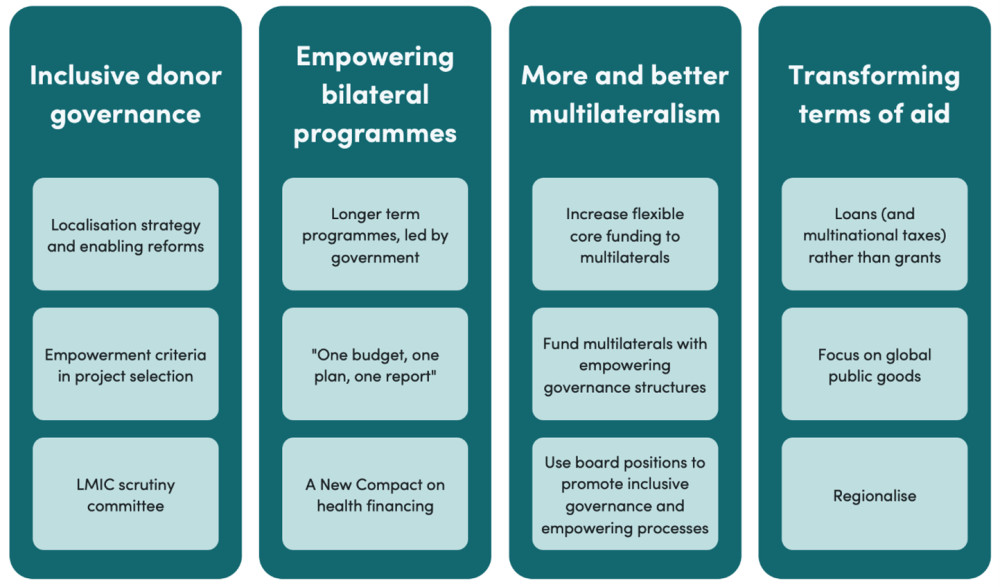
I recognise that—to an extent—I am a part of the power imbalance described in this blog. However, addressing this power imbalance requires constructive engagement from both sides. This blog therefore sets out to review the options for redistributing power from global health donors to governments and citizens of LMICs. It identifies four broad actions: more inclusive donor governance, empowering bilateral programmes, more and better multilateralism, and transforming the terms of aid (Figure 1).
Figure 1: Four broad options for redistributing power in global health
1. Build inclusive donor governance
Individual bilateral donors have two broad options to unilaterally redistribute power. Firstly, a donor can reform its own governance and policies. This could include a localisation strategy, with a commitment to shifting both the design and resources of projects to local decision-makers and implementers.
As USAID has found, a localisation strategy may not make much progress by itself and must be accompanied by other reforms. For instance, there are a range of policies that currently favour US contractors, such as on complexity and size of grants, rigidity of US budgeting, and risk management policies. Pro-localisation reforms could also include adding an “empowerment criteria” for choosing which specific projects to fund, alongside traditional criteria such as value for money. For oversight, a committee of LMIC experts and leaders should review progress on empowerment, with the right to access documents, interview civil servants, and inspect decision-making. This could operate in a similar manner to ICAI’s review of UK aid performance. How this committee is appointed will be challenging, but ambassadors from the top five to 10 recipient nations could contribute to the appointment process. This could be linked to my colleagues’ proposal of a “Real Assistance Committee” at the OECD DAC, which would include LMIC officials and hold each country accountable for appropriate standards of aid.
2. Develop empowering bilateral programmes
Secondly, donors can reform their bilateral programmes with specific countries, which make up approximately $18.3 billion (43 percent) of development assistance for health (see Table 1). This should be guided by the same principles as the Paris Declaration and Accra Agenda.
For example, aiming for longer term programmes that are led by national governments, aligned to national strategies, developing national institutions and capacity, and using national planning, financing, and delivery systems. Single donors can catalyse others to do the same, with the aim of following the mantra of “one budget, one plan, one report.” The minister of health would coordinate these donors behind an appropriate governance mechanism, such as a health developments partner forum. One specific approach is a New Compact on health financing, where LMICs countries set their own priorities, domestic financing is focused on the core essential services, and donors agree to support this, expand it, and to transition funding to more marginal services. This empowers governments both in terms of controlling priorities, but also in controlling core services.
3. More—and better—multilateralism
Beyond unilateral reform, donors can also act jointly through multilateral channels. This can be thought of in three parts: the UN system, including the World Health Organization (WHO) ($7.1 billion, 17 percent), the development banks such as the World Bank ($3.4 billion, 8 percent), and global health initiatives, especially the Global Fund and Gavi, which notably include a greater degree of philanthropic funding ($6.1 billion, 14 percent). Although predominantly Geneva- and DC-based, these mechanisms do include LMIC governments in their governance structures, and so, to an extent, decision-making is joint between donors and recipients. The ability of each multilateral agency to truly redistribute power depends on both its governance and funding arrangements. For example, WHO is directed by the World Health Assembly, using a “one country, one vote” system that is a relatively equal and democratic approach to tackling global challenges. This is in direct contrast to the World Bank, which has been criticised by the UN secretary general for giving donors more votes than recipients. Around 75 percent of WHO funding, however, is restricted by donors for specific projects that they define. This substantially distorts both the resources and whole agenda at WHO, undermining its democratic governance.
Therefore, there are opportunities to redistribute power by reforming the governance and financing systems of multilaterals. Indeed the World Health Assembly agreed in 2022 to seek to reduce this restricted funding to 50 percent by 2031.
Reforming multilateral institutions and financing may be a route to more democratic decision-making globally, but whether they empower countries also depends on how they spend their money within countries. The World Bank, for example, can claim to be empowering by substantially funding governments directly through grants or concessional loans. In contrast, the Future of Global Health Initiatives report found Gavi and the Global Fund financing mechanisms often fragment and distort local decision-making. Donors may therefore use their current board-level influence to direct multilaterals to adopt empowering processes, such as working through national priority-setting institutions and funding through government systems, rather than enforcing their own globally set priorities and using their own specific financing structures.
In summary, donors have three policy options at the multilateral level: allocate more core flexible funding to multilaterals; divert funding to multilateral mechanisms that have a more empowering governance structure; and use their power to reform multilateral governance, funding, and processes. As a successful example of what donors can do unilaterally, the UK is voluntarily providing £342 million of additional (and mostly flexible) core funding to WHO.
4. Transform the terms of global health aid
Beyond multilateralism, there are options to transform the underlying terms of global heath aid. Providing concessional loans, such as through the World Bank, tends to lead to a more empowering relationship, a greater use of government systems, and less conditions than the usual charitable model of grants.
Another option is internationally agreed taxes that go to a multilateral fund, which may reduce the sense of voluntary charitable giving, shifting the logic to entitlements based on redistributive justice. An example of this is the airline solidarity contribution that has contributed to Unitaid.
A third, and perhaps more radical option, is to “transition to sunset” all countries from direct aid, and shift aid resources solely to producing global public goods that benefit everyone, such as pandemic preparedness or investment in open access science. This is often the preferred approach of people who view aid as fundamentally disempowering and harmful to the political economy and democratic process in recipient countries. To be empowering, however, it still relies on an effective multilateral system to agree what the agenda is for global public goods and how to appropriately balance different country needs, which, as shown by the Pandemic Fund, is challenging. One intermediate option here is to promote regionalism and regional public goods rather than only global public goods, such as through the African Development Bank or Africa CDC, which may be better able to balance regional interests and decide regional priorities.
Conclusion
The power structures of global health are long overdue a reform. The policy options listed above won’t be right for each donor, nor are they all mutually compatible, but all donors should attempt to make progress on a selection of them over 2024. We should also be cognisant of the UN Secretary-General’s bold statement in 2019—“Power is not given, power is taken”—and recognise the limitations of this donor-focused set of policy options. LMIC leaders will surely identify their own mechanisms to readdress the power imbalances in global health.
With thanks to Ian Mitchell and Javier Guzman for comments on an earlier draft.
Postscript: Table 1: Percentage of development assistance for health through each channel
|
Channel |
$ (Billions) |
% |
|---|---|---|
|
Bilateral |
18.3 |
43% |
|
Philanthropy |
7.9 |
18% |
|
Multilateral – UN system |
7.1 |
17% |
|
Multilateral – Global Health Initiatives |
6.1 |
14% |
|
Multilateral – development banks |
3.4 |
8% |
Source: Author calculations based on Institute for Health Metrics and Evaluation (IHME). Financing Global Health. Seattle, WA: IHME, University of Washington, 2023. Available from http://vizhub.healthdata.org/fgh/
(Accessed 23rd April 2024)
Disclaimer
CGD blog posts reflect the views of the authors, drawing on prior research and experience in their areas of expertise. CGD is a nonpartisan, independent organization and does not take institutional positions.